Medical information
From the list below select the procedures you are interested in and find useful information about them.
Knee
Total Knee ReplacementUnicompartmental Arthroplasty and Tibial Osteotomy
Arthroscopic Meniscectomy
ACL reconstruction / PCL reconstruction
Hip
Minimally Invasive Total Hip ReplacementBack
Herniated Disc SurgeryLumbar Spinal Stenosis. Laminectomy
Shoulder
Arthroscopic Rotator Cuff RepairArthroscopic Shoulder Decompression
Hand
Carpal tunnel releaseFasciectomy for Dupuytren’s Contracture
Carpal tunnel release
Carpal Tunnel Syndrome
Introduction
Some people might think that carpal tunnel syndrome is a new condition of the information technology age, born from long hours of computer keyboarding. But carpal tunnel syndrome isn't new. Evidence of people experiencing signs and symptoms of carpal tunnel syndrome occurs in medical records dating back to the beginning of the 20th century.
Bounded by bones and ligaments, the carpal tunnel is a narrow passageway — about as big around as your thumb — located on the palm side of your wrist. This tunnel protects a main nerve to your hand and nine tendons that bend your fingers. Pressure placed on the nerve produces the numbness, pain and, eventually, hand weakness that characterize carpal tunnel syndrome.
Fortunately, for most people who develop carpal tunnel syndrome, proper treatment usually can relieve the pain and numbness and restore normal use of the wrists and hands.
Signs and symptoms
Carpal tunnel syndrome typically starts gradually with a vague aching in your wrist that can extend to your hand or forearm. Other common carpal tunnel syndrome symptoms include:
• Tingling or numbness in your fingers or hand, especially your thumb, index, middle or ring fingers, but not your little finger. This sensation often occurs while driving a vehicle or holding a phone or a newspaper or upon awakening. Many people "shake out" their hands to relieve their symptoms.
• Pain radiating or extending from your wrist up your arm to your shoulder or down into your palm or fingers, especially after forceful or repetitive use. This usually occurs on palm side of your forearm.
• A sense of weakness in your hands and a tendency to drop objects.
• A constant loss of feeling in some fingers. This can occur if the condition is advanced.
Causes
The cause of carpal tunnel syndrome is pressure on the median nerve. The median nerve is a mixed nerve, meaning it has a sensory function and also provides nerve signals to move your muscles (motor function). The median nerve provides sensation to your thumb, index finger, middle finger and the middle-finger side of the ring finger.
Pressure on the nerve can stem from anything that reduces the space for it in the carpal tunnel. Causes might include anything from bone spurs to the most common cause, which is swelling or thickening of the lining and lubricating layer (synovium) of the tendons in your carpal tunnel.
The exact cause of the swelling usually isn't known, but a variety of conditions and factors can play a role:
• Other health conditions. Some examples include rheumatoid arthritis, certain hormonal disorders — such as diabetes, thyroid disorders and menopause — fluid retention due to pregnancy, or deposits of amyloid, an abnormal protein produced by cells in your bone marrow.
• Repetitive use or injury. Repetitive flexing and extending of the tendons in the hands and wrists, particularly when done forcefully and for prolonged periods without rest, also can increase pressure within the carpal tunnel. Injury to your wrist can cause swelling that exerts pressure on the median nerve.
• Physical characteristics. It may be that your carpal tunnel is more narrow than average. Other less common causes include a generalized nerve problem or pressure on the median nerve at more than one location.
Risk factors
Some studies suggest that carpal tunnel syndrome can result from overuse or strain in certain job tasks that require a combination of repetitive, forceful and awkward or stressed motions of your hands and wrists. Examples of these include using power tools — such as chippers, grinders, chain saws or jackhammers — and heavy assembly line work, such as occurs in a meatpacking plant. Although repetitive computer use is commonly assumed to cause carpal tunnel syndrome, the scientific evidence for this association isn't definitive.
Although it's not clear which activities can cause carpal tunnel syndrome, if your work or hobbies are hand-intensive — involving a combination of awkward, repetitive wrist or finger motions, forceful pinching or gripping, and working with vibrating tools — you may be at higher risk of developing the condition.
Other risk factors include:
• Your sex. Women are three times as likely as men are to develop carpal tunnel syndrome. The incidence in women peaks after menopause, and the risk of carpal tunnel syndrome also increases in men during middle age.
• Heredity. You may be significantly more likely to develop carpal tunnel syndrome if close relatives have had the condition. Inherited physical characteristics, such as the shape of your wrist, may make you more susceptible.
• Certain health conditions. Conditions including some thyroid problems, diabetes, obesity and rheumatoid arthritis can increase your risk. Women who are pregnant, taking oral contraceptives or going through menopause also are at increased risk, most likely due to hormonal changes. Fluid retention may be a cause of carpal tunnel syndrome during pregnancy. Fortunately, carpal tunnel syndrome related to pregnancy almost always improves after childbirth. People who smoke cigarettes may experience worse symptoms and slower recovery from carpal tunnel syndrome than nonsmokers do.
When to seek medical advice
If signs and symptoms that you think might be due to carpal tunnel syndrome interfere with your normal activities — including sleep — and if they persist, see your doctor. If you leave the condition untreated, nerve and muscle damage can occur.
Screening and diagnosis
Your doctor will most likely want to review your signs and symptoms to find out where they're located. One diagnostic key is that the median nerve doesn't provide sensation to the little finger, so symptoms in that finger may indicate a different problem. Another clue is the timing of the symptoms. Typical times when you might experience symptoms due to carpal tunnel syndrome include while holding a phone or a newspaper, gripping a steering wheel, or waking up during the night.
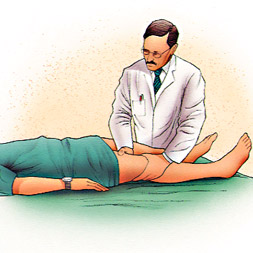
Your doctor will also want to test the feeling in your fingers and the strength of the muscles in your hand, because these can be affected by carpal tunnel syndrome. Pressure on the median nerve at the wrist, produced by either bending the wrist, tapping on the nerve or simply pressing on the nerve, can bring on the symptoms in many people.
If you have signs and symptoms of carpal tunnel syndrome, your doctor may recommend the following diagnostic tests:
• Electromyogram. Electromyography measures the tiny electrical discharges produced in muscles. A thin-needle electrode is inserted into the muscles your doctor wants to study. An instrument records the electrical activity in your muscle at rest and as you contract the muscle. This test can help determine if muscle damage has occurred.
• Nerve conduction study. In a variation of electromyography, two electrodes are taped to your skin. A small shock is passed through the median nerve to see if electrical impulses are slowed in the carpal tunnel.
These tests are also useful in checking for other conditions that might mimic carpal tunnel syndrome, such as a pinched nerve in your neck. Your doctor may recommend that you see a rheumatologist, neurologist, hand surgeon or neurosurgeon if your signs or symptoms indicate other medical disorders or a need for specialized treatment.
Treatment
Some people with mild symptoms of carpal tunnel syndrome can ease their discomfort by taking more frequent breaks to rest their hands and applying cold packs to reduce occasional swelling. If these techniques don't offer relief, carpal tunnel syndrome treatment options include wrist splinting, medications and surgery.
Nonsurgical therapy
Most people with carpal tunnel syndrome experience effective treatment with nonsurgical methods, including:
• Wrist splinting. A splint that holds your wrist still while you sleep can help relieve nighttime symptoms of tingling and numbness. Splinting is more likely to help you if you've had only mild to moderate symptoms for less than a year.
• Nonsteroidal anti-inflammatory drugs. NSAIDs may help relieve pain from carpal tunnel syndrome if you have an associated inflammatory condition. If no inflammatory condition is involved, NSAIDs are unlikely to help relieve your symptoms.
• Corticosteroids. Your doctor may inject your carpal tunnel with a corticosteroid, such as cortisone, to relieve your pain. Corticosteroids decrease inflammation, thus relieving pressure on the median nerve. Oral corticosteroids aren't as effective as corticosteroid injections for treating carpal tunnel syndrome.
Surgery
Generally, nonsurgical treatments are more effective if you have only mild nerve impairment. When the pain or numbness of carpal tunnel syndrome persists, surgery may be the best option.
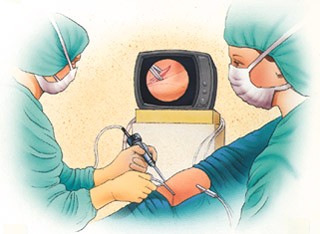
Your surgeon may use one of a few accepted techniques. But in all accepted surgical procedures, your doctor cuts the ligament pressing on your nerve. At times, surgery can be done using an endoscope, a telescope-like device with a tiny camera attached to it that allows your doctor to see inside your carpal tunnel and perform the surgery through small incisions in your hand or wrist. In other cases, surgery involves making an incision in the palm of your hand over the carpal tunnel and releasing the nerve.
Surgery usually results in marked improvement, but you may experience some residual numbness, pain, stiffness or weakness. Surveys of people who have undergone carpal tunnel release indicate that about 70 percent are completely or very satisfied with the outcome of their surgery. Some variables that are associated with lower levels of satisfaction include consuming more than two alcoholic drinks a day, smoking, lower mental and physical health status before surgery, and exposure to repetitive, forceful activity — but not including keyboard use.
After surgery, your doctor may tell you that limited use of your hand and wrist is OK within a few days. However, it may take from several weeks to as long as a few months before you have unrestricted use of your hand and wrist. If surgery appears to be the best alternative for relieving your symptoms or preventing further muscle atrophy, be sure to talk with your surgeon about the procedure that will work best for you and with your plans to return to your previous activity levels, both at work and at home.
If carpal tunnel syndrome results from an inflammatory arthritis, such as rheumatoid arthritis, then treating the underlying condition generally also reduces the carpal tunnel syndrome symptoms.
Carpal tunnel release
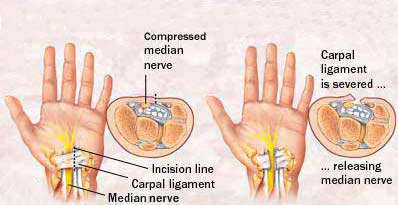
During carpal tunnel release, the transverse carpal tunnel ligament is severed to relieve pressure on the median nerve. The surgery may be done by making one incision on the palm side of the wrist, ...
Prevention
There are no proven strategies to prevent carpal tunnel syndrome, but to protect your hands from a variety of ailments, take the following precautions:
• Reduce your force and relax your grip. Most people use more force than needed to perform many tasks involving the hands. If your work involves a cash register, for instance, hit the keys softly. For prolonged handwriting, use a big pen with an oversized, soft grip adapter and free-flowing ink. This way you won't have to grip the pen tightly or press as hard on the paper.
• Take frequent breaks. Every 15 to 20 minutes give your hands and wrists a break by gently stretching and bending them. Alternate tasks when possible. If you use equipment that vibrates or that requires you to exert a great amount of force, taking breaks is even more important.
• Watch your form. Avoid bending your wrist all the way up or down. A relaxed middle position is best. If you use a keyboard, keep it at elbow height or slightly lower.
• Improve your posture. Incorrect posture can cause your shoulders to roll forward. When your shoulders are in this position, your neck and shoulder muscles are shortened, compressing nerves in your neck. This can affect your wrists, fingers and hands.
• Keep your hands warm. You're more likely to develop hand pain and stiffness if you work in a cold environment. If you can't control the temperature at work, put on fingerless gloves that keep your hands and wrists warm.
Self-care
Quick breaks, stretching, aspirin or other over-the-counter NSAIDs may relieve your symptoms temporarily.
You might also want to try wearing a wrist splint at night and avoid sleeping on your hands to help ease the pain or numbness in your wrists and hands. The splint should be snug but not tight. If pain, numbness or weakness recurs and persists, see your doctor.
Coping skills
If you experience chronic pain or can't use your hands as before, you may become depressed or experience low self-esteem. In addition, if your hand symptoms are caused or worsened by your current profession or leisure activities, you may face the tough decision of switching careers or giving up hobbies. You may also feel that you aren't actively contributing to your family if you can't drive a car or perform ordinary household tasks.
Support groups for people with carpal tunnel syndrome can help you find out more information about your condition plus offer advice and solace. Stress management and relaxation techniques also may help you deal with the psychological and emotional issues that may accompany carpal tunnel syndrome.
Complementary and alternative medicine
Yoga and other relaxation techniques may help with chronic pain that occurs with some muscle and joint conditions. Yoga postures designed for strengthening, stretching and balancing each joint in the upper body, as well as the upper body itself, may help reduce the pain and improve the grip strength of people with carpal tunnel syndrome.
Other options for treatment involve special types of physical therapy. Many of the methods used for c
arpal tunnel syndrome include:
• Heat
• Massage
• Water therapy (hydrotherapy)
You may have to experiment to find a treatment that works for you. Still, always check with your doctor before trying any complementary or alternative treatment.
Total Knee Replacement
Total Knee Replacement
General information
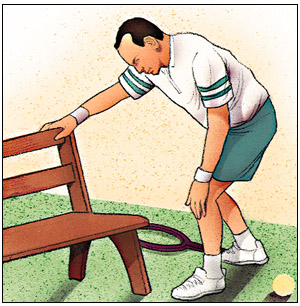
If your knee is severely damaged by arthritis or injury, it may be hard for you to perform simple activities such as walking or climbing stairs. You may even begin to feel pain while you're sitting or lying down.
If medications, changing your activity level and using walking supports are no longr helpful, you may want to consider total knee replacement surgery. By resurfacing your knee's damaged and worn surfaces, total knee replacement surgery can relieve your pain, correct your leg deformity and help you resume your normal activities.
One of the most important orthopaedic surgical advances of the twentieth century, knee replacement was first performed in 1968. Improvements in surgical materials and techniques since then have greatly increased its effectiveness. Approximately 300,000 knee replacements are performed each year in the United States.
Whether you have just begun exploring treatment options or have already decided with your orthopaedic surgeon to have total knee replacement surgery, this booklet will help you understand more about this valuable procedure.

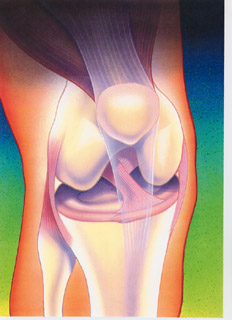
How the Normal Knee Works
The knee is the largest joint in the body. Nearly normal knee function is needed to perform routine everyday activities. The knee is made up of the lower end of the thigh bone (femur), which rotates on the upper end of the shin bone (tibia), and the knee cap (patella), which slides in a groove on the end of the femur. Large ligaments attach to the femur and tibia to provide stability. The long thigh muscles give the knee strength.
The joint surfaces where these three bones touch are covered with articular cartilage, a smooth substance that cushions the bones and enables them to move easily.
All remaining surfaces of the knee are covered by a thin, smooth tissue liner called the synovial membrane. This membrane releases a special fluid that lubricates the knee, reducing friction to nearly zero in a healthy knee.
Normally, all of these components work in harmony. But disease or injury can disrupt this harmony, resulting in pain, muscle weakness and less function.

Common Causes of Knee Pain and Loss of Knee Function
The most common cause of chronic knee pain and disability is arthritis. Osteoarthritis, rheumatoid arthritis and traumatic arthritis are the most common forms.
Osteoarthritis usually occurs after the age of 50 and often in an individual with a family history of arthritis. The cartilage that cushions the bones of the knee softens and wears away. The bones then rub against one another, causing knee pain and stiffness.
Rheumatoid Arthritis is a disease in which the synovial membrane becomes thickened and inflamed, producing too much synovial fluid that over-fills the joint space. This chronic inflammation can damage the cartilage and eventually cause cartilage loss, pain and stiffness.
Traumatic Arthritis can follow a serious knee injury. A knee fracture or severe tears of the knee's ligaments may damage the articular cartilage over time, causing knee pain and limiting knee function.

Is Total Knee Replacement for You?
The decision whether to have total knee replacement surgery should be a cooperative one between you, your family, your family physician and your orthopaedic surgeon. Your physician may refer you to an orthopaedic surgeon for a thorough evaluation to determine if you could benefit from this surgery. Alternatives to traditional total knee replacement surgery that your orthopaedic surgeon may discuss with you include a unicompartmental knee replacement or a minimally invasive knee replacement.
Reasons that you may benefit from total knee replacement commonly include:
• Severe knee pain that limits your everyday activities, including walking, going up and down stairs, and getting in and out of chairs. You may find it hard to walk more than a few blocks without significant pain and you may need to use a cane or walker.
• Moderate or severe knee pain while resting, either day or night
• Chronic knee inflammation and swelling that doesn't improve with rest or medications
• Knee deformity--a bowing in or out of your knee
• Knee stiffness--inability to bend and straighten your knee
• Failure to obtain pain relief from non-steroidal anti-inflammatory drugs. These medications, including aspirin and ibuprofen, often are most effective in the early stages of arthritis. Their effectiveness in controlling knee pain varies greatly from person to person. These drugs may become less effective for patients with severe arthritis.

• Inability to tolerate or complications from pain medications
• Failure to substantially improve with other treatments such as cortisone injections, physical therapy, or other surgeries
Most patients who undergo total knee replacement are age 60 to 80, but orthopaedic surgeons evaluate patients individually. Recommendations for surgery are based on a patient's pain and disability, not age. Total knee replacements have been performed successfully at all ages, from the young teenager with juvenile arthritis to the elderly patient with degenerative arthritis.
The Orthopaedic Evaluation
The orthopaedic evaluation consists of several components:
• A medical history, in which your orthopaedic surgeon gathers information about your general health and asks you about the extent of your knee pain and your ability to function
• A physical examination to assess your knee motion, stability, strength and overall leg alignment
• X-rays to determine the extent of damage and deformity in your knee
• Occasionally blood tests, a Magnetic Resonance Image (MRI) or a bone scan may be needed to determine the condition of the bone and soft tissues of your knee.
•
Your orthopaedic surgeon will review the results of your evaluation with you and discuss whether total knee replacement would be the best method to relieve your pain and improve your function. Other treatment options--including medications, injections, physical therapy, or other types of surgery--also will be discussed and considered.
Your orthopaedic surgeon also will explain the potential risks and complications of total knee replacement, including those related to the surgery itself and those that can occur over time after your surgery.

Realistic Expectations About Knee Replacement Surgery
An important factor in deciding whether to have total knee replacement surgery is understanding what the procedure can and can't do.
More than 90 percent of individuals who undergo total knee replacement experience a dramatic reduction of knee pain and a significant improvement in the ability to perform common activities of daily living. But total knee replacement won't make you a super-athlete or allow you to do more than you could before you developed arthritis.
Following surgery, you will be advised to avoid some types of activity, including jogging and high impact sports, for the rest of your life.
With normal use and activity, every knee replacement develops some wear in its plastic cushion. Excessive activity or weight may accelerate this normal wear and cause the knee replacement to loosen and become painful. With appropriate activity modification, knee replacements can last for many years.

Preparing for Surgery
Medical Evaluation
If you decide to have total knee replacement surgery, you may be asked to have a complete physical by your family physician several weeks before surgery to assess your health and to rule out any conditions that could interfere with your surgery.
Tests
Several tests-such as blood samples, a cardiogram and a urine sample-may be needed to help your orthopaedic surgeon plan your surgery.
Preparing Your Skin and Leg
Your knee and leg should not have any skin infections or irritation. Your lower leg should not have any chronic swelling. Contact your orthopaedic surgeon prior to surgery if either of these conditions is present for a program to best prepare your skin for surgery.
Blood Donation
You may be advised to donate your own blood prior to the surgery. It will be stored in the event you need blood after your surgery.
Medications
Tell your orthopaedic surgeon about the medications you are taking. He or she will tell you which medications you should stop taking and which you should continue to take before surgery.
Dental Evaluation
Although the incidence of infection after knee replacement is very low, an infection can occur if bacteria enter your bloodstream. Treatment of significant dental diseases (including tooth extractions and periodontal work) should be considered before your total knee replacement surgery.
Urinary Evaluations
A preoperative urological evaluation should be considered for individuals with a history of recent or frequent urinary infections. For older men with prostate disease, required treatment should be considered prior to knee replacement surgery.
Social Planning
Though you will be able to walk on crutches or a walker soon after surgery, you will need help for several weeks with such tasks as cooking, shopping, bathing and doing laundry. If you live alone, your surgeon's office and a social worker or a discharge planner at the hospital can help you make advance arrangements to have someone assist you at home. They also can help you arrange for a short stay in an extended care facility during your recovery, if this option works best for you.
Home Planning
Several suggestions can make your home easier to navigate during your recovery. Consider:
• Safety bars or a secure handrail in your shower or bath
• Secure handrails along your stairways
• A stable chair for your early recovery with a firm seat cushion (height of 18-20 inches), a firm back, two arms, and a footstool for intermittent leg elevation
• A toilet seat riser with arms, if you have a low toilet
• A stable shower bench or chair for bathing
• Removing all loose carpets and cords

• A temporary living space on the same floor, because walking up or down stairs will be more difficult during your early recovery
Your Surgery
You will most likely be admitted to the hospital on the day of your surgery. After admission, you will be evaluated by a member of the anesthesia team. The most common types of anesthesia are general anesthesia, in which you are asleep throughout the procedure, and spinal or epidural anesthesia, in which you are awake but your legs are anesthetized. The anesthesia team will determine which type of anesthesia will be best for you with your input.
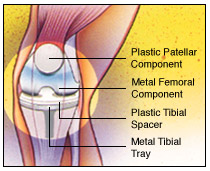
The procedure itself takes about two hours. Your orthopaedic surgeon will remove the damaged cartilage and bone and then position the new metal and plastic joint surfaces to restore the alignment and function of your knee.
Many different types of designs and materials are currently used in total knee replacement surgery. Nearly all of them consist of three components: the femoral component (made of a highly polished strong metal), the tibial component (made of a durable plastic often held in a metal tray), and the patellar component (also plastic).
After surgery, you will be moved to the recovery room, where you will remain for one to two hours while your recovery from anesthesia is monitored. After you awaken, you will be taken to your hospital room.
Your Stay in the Hospital
You will most likely stay in the hospital for several days. After surgery, you will feel some pain, but medication will be given to you to make you feel as comfortable as possible. Pain management is an important part of your recovery, so talk with your surgeon if postoperative pain becomes a problem. Walking and knee movement are important to your recovery and will begin immediately after your surgery.
To avoid lung congestion after surgery, you should breathe deeply and cough frequently to clear your lungs.
Your orthopaedic surgeon may prescribe one or more measures to prevent blood clots and decrease leg swelling, such as special support hose, inflatable leg coverings (compression boots) and blood thinners.
To restore movement in your knee and leg, your surgeon may use a knee support that slowly moves your knee while you are in bed. The device, called a continuous passive motion (CPM) machine, decreases leg swelling by elevating your leg and improves your venous circulation by moving the muscles of your leg.
Foot and ankle movement also is encouraged immediately following surgery to increase blood flow in your leg muscles to help prevent leg swelling and blood clots. Most patients begin exercising their knee the day after surgery. A physical therapist will teach you specific exercises to strengthen your leg and restore knee movement to allow walking and other normal daily activities soon after your surgery.

Possible Complications After Surgery
The complication rate following total knee replacement is low. Serious complications, such as a knee joint infection, occur in less than 2 percent of patients. Major medical complications such as heart attack or stroke occur even less frequently. Chronic illnesses may increase the potential for complications. Although uncommon, when these complications occur, they can prolong or limit your full recovery.
Blood clots in the leg veins are the most common complication of knee replacement surgery. Your orthopaedic surgeon will outline a prevention program, which may include periodic elevation of your legs, lower leg exercises to increase circulation, support stockings and medication to thin your blood.
Although implant designs and materials as well as surgical techniques have been optimized, wear of the bearing surfaces or loosening of the components may occur. Additionally, although an average of 115 degrees of motion is generally anticipated after surgery, scarring of the knee can occasionally occur and motion may be more limited. This is particularly true in patients with limited motion before surgery. Finally, while rare, injury to the nerves or blood vessels around the knee can occur during surgery.
Discuss your concerns thoroughly with your orthopaedic surgeon prior to surgery.
Your Recovery at Home
The success of your surgery also will depend on how well you follow your orthopaedic surgeon's instructions at home during the first few weeks after surgery.
Wound Care
You will have stitches or staples running along your wound or a suture beneath your skin on the front of your knee. The stitches or staples will be removed several weeks after surgery. A suture beneath your skin will not require removal.
Avoid soaking the wound in water until the wound has thoroughly sealed and dried. The wound may be bandaged to prevent irritation from clothing or support stockings.
Diet
Some loss of appetite is common for several weeks after surgery. A balanced diet, often with an iron supplement, is important to promote proper tissue healing and restore muscle strength.
Activity
Exercise is a critical component of home care, particularly during the first few weeks after surgery. You should be able to resume most normal activities of daily living within three to six weeks following surgery. Some pain with activity and at night is common for several weeks after surgery. Your activity program should include:
• A graduated walking program to slowly increase your mobility, initially in your home and later outside
• Resuming other normal household activities, such as sitting and standing and walking up and down stairs
• Specific exercises several times a day to restore movement and strengthen your knee. You probably will be able to perform the exercises without help, but you may have a physical therapist help you at home or in a therapy center the first few weeks after surgery.
Driving usually begins when your knee bends sufficiently so you can enter and sit comfortably in your car and when your muscle control provides adequate reaction time for braking and acceleration. Most individuals resume driving about four to six weeks after surgery.
Avoiding Problems After Surgery
Blood Clot Prevention
Follow your orthopaedic surgeon's instructions carefully to minimize the potential of blood clots that can occur during the first several weeks of your recovery.
Warning signs of possible blood clots in your leg include:
• Increasing pain in your calf
• Tenderness or redness above or below your knee
• Increasing swelling in your calf, ankle and foot
Warning signs that a blood clot has traveled to your lung include:
• Sudden increased shortness of breath
• Sudden onset of chest pain
• Localized chest pain with coughing
Notify your doctor immediately if you develop any of these signs.
Preventing Infection
The most common causes of infection following total knee replacement surgery are from bacteria that enter the bloodstream during dental procedures, urinary tract infections, or skin infections. These bacteria can lodge around your knee replacement and cause an infection.
For the first two years after your knee replacement, you must take preventive antibiotics before dental or surgical procedures that could allow bacteria to enter your bloodstream. After two years, talk to your orthopaedist and your dentist or urologist to see if you still need preventive antibiotics before any scheduled procedures.
Warning signs of a possible knee replacement infection are:
• Persistent fever (higher than 100 degrees orally)
• Shaking chills
• Increasing redness, tenderness or swelling of the knee wound
• Drainage from the knee wound
• Increasing knee pain with both activity and rest
Notify your doctor immediately if you develop any of these signs.
Avoiding Falls
A fall during the first few weeks after surgery can damage your new knee and may result in a need for further surgery. Stairs are a particular hazard until your knee is strong and mobile. You should use a cane, crutches, a walker, hand rails or someone to help you until you have improved your balance, flexibility and strength.
Your surgeon and physical therapist will help you decide what assistive aides will be required following surgery and when those aides can safely be discontinued.
How Your New Knee Is Different
You may feel some numbness in the skin around your incision. You also may feel some stiffness, particularly with excessive bending activities. Improvement of knee motion is a goal of total knee replacement, but restoration of full motion is uncommon. The motion of your knee replacement after surgery is predicted by the motion of your knee prior to surgery. Most patients can expect to nearly fully straighten the replaced knee and to bend the knee sufficiently to go up and down stairs and get in and out of a car. Kneeling is usually uncomfortable, but it is not harmful. Occasionally, you may feel some soft clicking of the metal and plastic with knee bending or walking. These differences often diminish with time and most patients find these are minor, compared to the pain and limited function they experienced prior to surgery.
Your new knee may activate metal detectors required for security in airports and some buildings. Tell the security agent about your knee replacement if the alarm is activated.

After surgery, make sure you also do the following:
• Participate in regular light exercise programs to maintain proper strength and mobility of your new knee.
• Take special precautions to avoid falls and injuries. Individuals who have undergone total knee replacement surgery and suffer a fracture may require more surgery.
• Notify your dentist that you had a knee replacement. You should be given antibiotics before all dental surgery for the rest of your life.
• See your orthopaedic surgeon periodically for a routine follow-up examination and X-rays, usually once a year.
Your orthopaedic surgeon is a medical doctor with extensive training in the diagnosis and nonsurgical and surgical treatment of the musculoskeletal system, including bones, joints, ligaments, tendons, muscles and nerves.
Unicompartmental Arthroplasty and Tibial Osteotomy
Osteotomy and Unicompartmental Knee Arthroplasty
Total joint replacement (arthroplasty) is a common and very successful surgery for people with degenerative arthritis (osteoarthritis) of the knee. Two other surgeries can also restore knee function and significantly diminish osteoarthritis pain in carefully selected patients. If osteoarthritis damage to your knee meets certain qualifications, a doctor may recommend either osteotomy or unicompartmental knee arthroplasty (UKA).
Osteoarthritis damage to the knee
A normal knee glides smoothly because articular cartilage covers the ends of the bones that form joints. Osteoarthritis damages the cartilage, progressively wearing it away. The ends of the bones become rough like pieces of sandpaper. Damaged cartilage can cause the joint to "stick" or lock when you use it. Your knee may get painful, stiff and lose range of motion. See your doctor to diagnose osteoarthritis.
Provide your complete medical history including detailed descriptions of osteoarthritis symptoms and when they began. Have you tried nonsurgical treatments such as rest, weight loss and nonsteroidal anti-inflammatory medication for pain? Does it hurt too much to get dressed, bathe or walk up stairs? The doctor will check your knee's range of motion, ligament stability and angular deformity. He or she will observe your knees while you stand and walk, and examine your hips, feet and ankles. Both knees will probably be X-rayed.
Your doctor's recommendation of a surgical procedure for osteoarthritis knee repair depends in part upon how it is damaged. The knee has three joints (compartments), any or all of which can be impacted by osteoarthritis:
• The inside (medial) compartment (medial tibial plateau and medial femoral condyle) is most commonly involved, producing a bowleg (genu varum) deformity.
• The outside (lateral) compartment (lateral tibial plateau and lateral femoral condyle) is sometimes involved in women or obese people, producing a knock-knee (genu valgum) deformity.
• The kneecap (patellofemoral) compartment (patella and femoral trochlear notch) may also develop osteoarthritis.
If you have early stage arthritis confined to one part of the knee, your doctor may recommend osteotomy or UKA.
Osteotomy
Osteotomy may be appropriate if you are younger than age 60, active or overweight. There must also be uneven damage to the joint, correctable deformity and no inflammation. The surgeon reshapes the shinbone (tibia) or thighbone (femur) to improve your knee's alignment. The healthy bone and cartilage is realigned to compensate for the damaged tissue. Knee osteotomy surgically repositions the joint, realigning the mechanical axis of the limb away from the diseased area. This lets your knee glide freely and carry weight evenly on a more normal compartment.
• Proximal tibial valgus osteotomy treats arthritis of the medial compartment, correcting a knee that angles inward (varus deformity).
• Distal femoral varus osteotomy treats arthritis of the lateral compartment, correcting a knee that angles outward (valgus deformity).
The doctor may use one of several techniques to hold the joint in place (i.e., immobilization with a cast, staples or internal plate devices).
Outcome: Osteotomy relieves pain and may delay the progression of osteoarthritis. Cosmetically, the knee may not look symmetrical after osteotomy. There's a chance you will eventually need TKA, which can be a more technically challenging procedure after you've had an osteotomy. Infections and other complications are possible. Depending upon how quickly you heal, you will need to walk with crutches for 1-3 months. After that you begin rehabilitative leg strengthening and walking exercises. You may be able to resume your full activities after 3-6 months.
Unicompartmental knee arthroplasty
Unicompartmental knee arthroplasty (UKA) may be appropriate if you are age 60 or older, not obese and relatively sedentary. Among other specific qualifications, your knee must have:
• An intact anterior cruciate ligament (ACL).
• No significant inflammation.
• No damage to the other compartments, calcification of cartilage or dislocation.
Your doctor will verify that your knee meets the requirements when he or she begins the surgery. (Note: If your knee does not meet the qualifications, you may need TKA.) The surgeon removes diseased bone and puts an implant (prosthesis) in its place. The two small replacement parts are secured to the rest of your knee. You can get UKA surgery on both knees at the same time if you need it.
Outcome: UKA aleviates pain and may delay the need for TKA. You get better joint motion and function because the procedure preserves both cruciate ligaments and other healthy parts of the knee. You also keep the bone stock in the kneecap joint and the other compartment, which can be helpful if you ever need conversion to TKA in the future. Complications are rare, but the new joint could develop an infection or slip out of place after surgery. For these reasons, your doctor may want to see you for follow-up visits after surgery. You will have to do range of motion and other physical therapy exercises to rehabilitate your knee. Recovery from UKA is faster than from TKA or osteotomy.
Although UKA was a controversial procedure when it was first introduced about 30 years ago, success rates have improved thanks to precise patient selection, refined surgical techniques and improved implant design. UKA has a higher initial success rate and fewer complications compared with osteotomy. Other advantages include less blood loss during surgery and cheaper cost.
Arthroscopic Meniscectomy
Knee Arthroscopy
If you have persistent pain, catching, or swelling in your knee, a procedure known as arthroscopy may help relieve these problems.
Arthroscopy allows an orthopaedic surgeon to diagnose and treat knee disorders by providing a clear view of the inside of the knee with small incisions, utilizing a pencil-sized instrument called an arthroscope. The scope contains optic fibers that transmit an image of your knee through a small camera to a television monitor. The TV image allows the surgeon to thoroughly examine the interior of your knee and determine the source of your problem. During the procedure, the surgeon also can insert surgical instruments through other small incisions in your knee to remove or repair damaged tissues.
Modern or contemporary arthroscopy of the knee was first performed in the late 1960s. With improvements of arthroscopes and higher-resolution cameras, the procedure has become highly effective for both the accurate diagnosis and proper treatment of knee problems. Today, arthroscopy is one of the most common orthopaedic procedures in the United States.
Whether you have just begun exploring treatment options for your problem knee or have already decided, with your orthopaedic surgeon, to have an arthroscopy, this booklet will help you understand more about this valuable procedure.
How the Normal Knee Works
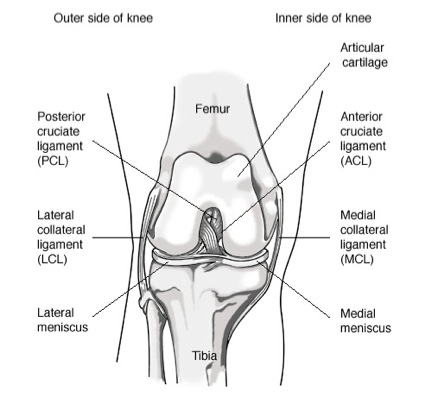
The knee is the largest joint in the body, and one of the most easily injured. It is made up of the lower end of the thigh bone (femur), the upper end of the shin bone (tibia), and the knee cap (patella), which slides in a groove on the end of the femur. Four bands of tissue, the anterior and posterior cruciate ligaments, and the medial and lateral collateral ligaments connect the femur and the tibia and provide joint stability. Strong thigh muscles give the knee strength and mobility.
The surfaces where the femur, tibia and patella touch are covered with articular cartilage, a smooth substance that cushions the bones and enables them to glide freely. Semicircular rings of tough fibrous-cartilage tissue called the lateral and medial menisci act as shock absorbers and stabilizers.
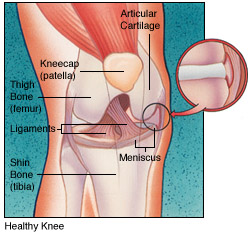
The bones of the knee are surrounded by a thin, smooth tissue capsule lined by a thin synovial membrane which releases a special fluid that lubricates the knee, reducing friction to nearly zero in a healthy knee.
Knee Problems
Normally, all parts of the knee work together in harmony. But sports, work injuries, arthritis, or weakening of the tissues with age can cause wear and inflammation, resulting in pain and diminished knee function.
Arthroscopy can be used to diagnose and treat many of these problems:
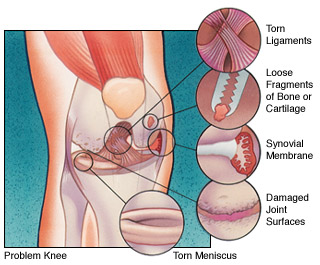
• Loose fragments of bone or cartilage.
• Damaged joint surfaces or softening of the articular cartilage known as chondromalacia.
• Inflammation of the synovial membrane, such as rheumatoid or gouty arthritis.
• Abnormal alignment or instability of the kneecap.
• Torn ligaments including the anterior and posterior cruciate ligaments.

By providing a clear picture of the knee, arthroscopy can also help the orthopaedic surgeon decide whether other types of reconstructive surgery would be beneficial.
Is Arthroscopy for You?
Your family physician can refer you to an orthopaedic surgeon for an evaluation to determine whether you could benefit from arthroscopy.
Signs that you may be a candidate for this procedure include swelling, persistent pain, catching, giving-way, and loss of confidence in your knee. When other treatments such as the regular use of medications, knee supports, and physical therapy have provided minimal or no improvement, you may benefit from arthroscopy.
Most arthroscopies are performed on patients between the ages of 20 and 60, but patients younger than 10 years and older than 80 years have benefited from the procedure.
The Orthopaedic Knee Evaluation
The orthopaedic knee evaluation consists of three components:
• A medical history, in which your orthopaedic surgeon gathers information about your general health and asks you about your symptoms.
• A physical examination to assess your knee motion and stability, muscle strength and overall leg alignment.
• X-rays to evaluate the bones of your knee. Your orthopaedic surgeon may also arrange for you to have an MRI to provide more information about the soft tissues of your knee. An MRI uses magnetic sound waves to create images. They are not X-rays. Blood tests may be obtained to determine if you have arthritis.
Your orthopaedic surgeon will review the results of your evaluation with you and discuss whether arthroscopy would be the best method to further diagnose and treat your knee problem. Other treatment options, such as medications or other surgical procedures also will be discussed and considered.
Your orthopaedic surgeon will explain the potential risks and complications of knee arthroscopy, including those related to the surgery itself and those that can occur after your surgery.
Preparing for Surgery
If you decide to have arthroscopy, you may be asked to have a complete physical with your family physician before surgery to assess your health and to rule out any conditions that could interfere with your surgery.
Before surgery, tell your orthopaedic surgeon about any medications that you are taking. You will be informed which medications you should stop taking before surgery.
Tests, such as blood samples or a cardiogram, may be ordered by your orthopaedic surgeon to help plan your procedure.
Your Arthroscopic Knee Surgery
Almost all arthroscopic knee surgery is done on an outpatient basis. Your hospital or surgery center will contact you about the specific details for your surgery, but usually you will be asked to arrive at the hospital an hour or two prior to your surgery. Do not eat or drink anything after midnight the night before your surgery.
After arrival, you will be evaluated by a member of the anesthesia team. Arthroscopy can be performed under local, regional, or general anesthesia. Local anesthesia numbs your knee, regional anesthesia numbs you below your waist, and general anesthesia puts you to sleep. The anesthesiologist will help you determine which would be the best for you.
If you have local or regional anesthesia, you may be able to watch the procedure on a TV screen, if you wish.
The orthopaedic surgeon will make a few small incisions in your knee. A sterile solution will be used to fill the knee joint and rinse away any cloudy fluid, providing a clear view of your knee.
The surgeon will then insert the arthroscope to properly diagnose your problem, using the TV image to guide the arthroscope. If surgical treatment is needed, the surgeon can use a variety of small surgical instruments (e.g., scissors, clamps, motorized shavers, or lasers) through another small incision. This part of the procedure usually lasts 45 minutes to 1 1/2 hours.
Common treatments with knee arthroscopy include:
• Removal or repair of torn meniscal cartilage.
• Reconstruction of a torn cruciate ligament.
• Trimming of torn pieces of articular cartilage.
• Removal of loose fragments of bone or cartilage.
• Removal of inflamed synovial tissue.
At the conclusion of your surgery, the surgeon may close your incisions with a suture or paper tape and cover them with a bandage.
You will be moved to the recovery room. Usually, you will be ready to go home in one or two hours. You should have someone with you to drive you home.
Your Recovery at Home
Recovery from knee arthroscopy is much faster than recovery from traditional open knee surgery. Still, it is important to follow your orthopaedic surgeon's instructions carefully after you return home. You should ask someone to check on you that evening.
Swelling Keep your leg elevated as much as possible for the first few days after surgery. Apply ice as recommended by your orthopaedic surgeon to relieve swelling and pain.
Dressing Care: You will leave the hospital with a dressing covering your knee. You may remove the dressing the day after surgery. You may shower, but should avoid directing water at the incisions. Do not soak in a tub. Keep your incisions clean and dry.
Your orthopaedic surgeon will see you in the office a few days after surgery to check your progress, review the surgical findings, and begin your postoperative treatment program.
Bearing Weight: After most arthroscopic surgeries, you can walk unassisted but your orthopaedic surgeon may advise you to use crutches, a cane, or a walker for a period of time after surgery. You can gradually put more weight on your leg as your discomfort subsides and you regain strength in your knee. Your surgeon may allow you to drive after a week.
Exercises to Strengthen Your Knee: you should exercise your knee regularly for several weeks following surgery to strengthen the muscles ofyour leg and knee. A physical therapist may help you with your exercise program if your orthopaedic surgeon recommends specific exercises.
Medications: your orthopaedic surgeon may prescribe antibiotics to help prevent an infection and pain medication to help relieve discomfort following your surgery.
Complications: potential postoperative problems with knee arthroscopy include infection, blood clots, and an accumulation of blood in the knee. These occur infrequently and are minor and treatable.

Warning Signs
Call your orthopaedic surgeon immediately if you experience any of the following:
• Fever.
• Chills.
• Persistent warmth or redness around the knee.
• Persistent or increased pain.
• Significant swelling in your knee.
• Increasing pain in your calf muscle.
• Shortness of breath or chest pain.
Reasonable Expectations After Arthroscopic Surgery
Although arthroscopy can be used to treat many problems, you may have some activity limitations even after recovery. The outcome of your surgery will often be determined by the degree of injury or damage found in your knee. For example, if you damage your knee from jogging and the smooth articular cushion of the weight-bearing portion of the knee has worn away completely, then full recovery may not be possible. You may be advised to find a low-impact alternative form of exercise. An intercollegiate or professional athlete often sustains the same injury as a weekend recreational athlete, but the potential for recovery may be improved by the over-development of knee muscles. Physical exercise and rehabilitation will play an important role in your final outcome. A formal physical therapy program also may add something to your final result.
A return to intense physical activity should only be done under the direction of your surgeon.
It is reasonable to expect that by six to eight weeks you should be able to engage in most of your former physical activities as long as they do not involve significant weight-bearing impact. Twisting maneuvers may have to be avoided for a longer time.
If your job involves heavy work, such as a construction laborer, you may require more time to return to your job than if you have a sedentary job.

Your orthopaedic surgeon is a medical doctor with extensive training in the diagnosis and nonsurgical and surgical treatment of the musculoskeletal system, including bones, joints, ligaments, tendons, muscles, and nerves.
ACL reconstruction / PCL reconstruction
Price
Knee Ligament Injuries
In 2003 more than 9.5 million people visited orthopaedic surgeons because of knee problems. (Source: National Center for Health Statistics; Centers for Disease Control and Prevention; 2003 National Ambulatory Medical Care Survey.) The knee is the largest joint in the body and is vital to movement. Two sets of ligaments in the knee give it stability: the cruciate and the collateral ligaments.
Cruciate ligaments
The cruciate ligaments are located inside the knee joint and connect the thighbone (femur) to the shinbone (tibia). They are made of many strands and function like short ropes that hold the knee joint tightly in place when the leg is bent or straight. This stability is needed for proper knee joint movement.
The name, cruciate, derives from the word crux, meaning cross, and crucial. The cruciate ligaments not only lie inside the knee joint, they crisscross each other to form an "x". The cruciate ligament located toward the front of the knee is the anterior cruciate ligament (ACL), and the one located toward the rear of the knee is called the posterior cruciate ligament (PCL).
ACL injuries
The ACL prevents the shinbone from sliding forwards beneath the thighbone. The ACL can be injured in several ways:
• Changing direction rapidly
• Slowing down when running
• Landing from a jump
• Direct contact, such as in a football tackle
Recognizing an ACL injury
If you injure your ACL, you may not feel any pain immediately. However, you might hear a popping noise and feel your knee give out from under you. Within 2 to 12 hours, the knee will swell, and you will feel pain when you try to stand. Apply ice to control swelling and elevate your knee until you can see an orthopaedic surgeon.
If you walk or run on an injured ACL, you can damage the cushioning cartilage in the knee. For example, you may plant the foot and turn the body to pivot, only to have the shinbone stay in place as the thighbone above it moves with the body.
Diagnosing an ACL injury
A diagnosis of ACL injury is based on a thorough physical examination of the knee. The exam may include several tests to see if the knee stays in the proper position when pressure is applied from different directions. Your orthopaedist may order an X-ray and MRI (magnetic resonance imaging) or, in some cases, arthroscopic inspection.
A partial tear of the ACL may or may not require surgical treatment. A complete tear is more serious. Complete tears, especially in younger athletes, may require reconstruction.
Treating ACL tears
Both nonoperative and operative treatment choices are available.
Nonoperative treatment:
• May be used because of a patient's age or overall low activity level.
• May be recommended if the overall stability of the knee seems good.
• Involves a treatment program of muscle strengthening, often with the use of a brace to provide stability.
• Operative treatment (either arthroscopic or open surgery): Uses a strip of tendon, usually taken from the patient's knee (patellar tendon) or hamstring muscle, that is passed through the inside of the joint and secured to the thighbone and shinbone.
• Is followed by an exercise and rehabilitation program to strengthen the muscles and restore full joint mobility.
PCL injuries
The posterior cruciate ligament, or PCL, is not injured as frequently as the ACL. PCL sprains usually occur because the ligament was pulled or stretched too far, a blow to the front of the knee, or a simple misstep.
PCL injuries disrupt knee joint stability because the shinbone can sag backwards. The ends of the thighbone and shinbone rub directly against each other, causing wear and tear to the thin, smooth articular cartilage. This abrasion may lead to arthritis in the knee.
Treating PCL injuries
Patients with PCL tears often do not have symptoms of instability in their knees, so surgery is not always needed. Many athletes return to activity without significant impairment after completing a prescribed rehabilitation program.
However, if the PCL injury pulls a piece of bone out of the top of the shinbone, surgery is needed to reattach the ligament. Knee function after this surgery is often quite good.
Collateral ligaments
The collateral ligaments are located at the inner side and outer side of the knee joint. The medial collateral ligament (MCL) connects the thighbone to the shinbone and provides stability to the inner side of the knee. The lateral collateral ligament (LCL) connects the thighbone to the other bone in the lower portion of your leg (fibula) and stabilizes the outer side.
Injuries to the MCL are usually caused by contact on the outside of the knee and are accompanied by sharp pain on the inside of the knee. The LCL is rarely injured.
Collateral ligament injuries
If the medial collateral ligament (MCL) has a small partial tear, conservative treatment usually works. Remember the acronym RICE: Rest, Ice, Compression, Elevation.
Rest the knee to give the ligament time to heal. Ice can be applied two or three times a day for 15 to 20 minutes each time.
Compress the injury to limit swelling. You may have to wear a bandage or brace for a while.
Elevate the knee whenever possible.
You should also consult your physician about a course of rehabilitation exercises for good healing.
If the collateral ligament is completely torn or torn in such a way that ligament fibers cannot heal, you may need surgery. Repair may bring good results, with a return to good knee stability. After satisfactory rehabilitation, many people resume their previous levels of activity.
A rehabilitation plan is needed if you have a cruciate or collateral ligament injury. Most rehabilitation plans include:
• Passive range-of-motion exercises designed to restore flexibility.
• Braces to control joint movement.
• Exercises to strengthen the quadriceps muscles in the front of the thigh. (Muscle strength is needed to provide the knee joint with as much support and stability as possible when weight is placed on it.)
• Additional exercises on a high-seat exercise bicycle, followed by more strenuous quadriceps exercise.
Your progress and the ability of the knee to function as a normal knee will determine how long you must use crutches and a brace.
Minimally Invasive Total Hip Replacement
Whether you have just begun exploring treatment options or have already decided with your orthopaedic surgeon to undergo hip replacement surgery, this information will help you understand the benefits and limitations of this orthopaedic treatment. You'll learn how a normal hip works and the causes of hip pain, what to expect from hip replacement surgery and what exercises and activities will help restore your mobility and strength and enable you to return to everyday activities.
If your hip has been damaged by arthritis, a fracture or other conditions, common activities such as walking or getting in and out of a chair may be painful and difficult. Your hip may be stiff and it may be hard to put on your shoes and socks. You may even feel uncomfortable while resting.
If medications, changes in your everyday activities, and the use of walking aids such as a cane are not helpful, you may want to consider hip replacement surgery. By replacing your diseased hip joint with an artificial joint, hip replacement surgery can relieve your pain, increase motion, and help you get back to enjoying normal, everyday activities.
First performed in 1960, hip replacement surgery is one of the most important surgical advances of the last century. Since then, improvements in joint replacement surgical techniques and technology have greatly increased the effectiveness of this surgery. Today, more than 193,000 total hip replacements are performed each year in the United States. Similar surgical procedures are performed on other joints, including the knee, shoulder, and elbow.
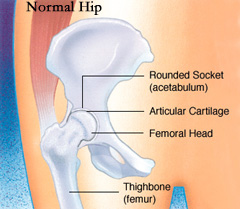
How the normal hip works
The hip is one of your body's largest weight-bearing joints. It consists of two main parts: a ball (femoral head) at the top of your thighbone (femur) that fits into a rounded socket (acetabulum) in your pelvis. Bands of tissue called ligaments (hip capsule) connect the ball to the socket and provide stability to the joint.
The bone surfaces of your ball and socket have a smooth durable cover of articular cartilage that cushions the ends of the bones and enables them to move easily.
A thin, smooth tissue called synovial membrane covers all remaining surfaces of the hip joint. In a healthy hip, this membrane makes a small amount of fluid that lubricates and almost eliminates friction in your hip joint.
Normally, all of these parts of your hip work in harmony, allowing you to move easily and without pain.
Common causes of hip pain and loss of hip mobility
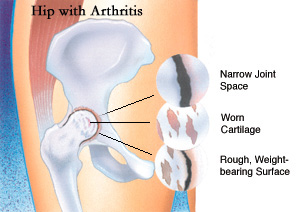
The most common cause of chronic hip pain and disability is arthritis. Osteoarthritis, rheumatoid arthritis, and traumatic arthritis are the most common forms of this disease.
Osteoarthritis usually occurs after age 50 and often in an individual with a family history of arthritis. It may be caused or accelerated by subtle irregularities in how the hip developed. In this form of the disease, the articular cartilage cushioning the bones of the hip wears away. The bones then rub against each other, causing hip pain and stiffness.
Rheumatoid Arthritis is an autoimmune disease in which the synovial membrane becomes inflamed, produces too much synovial fluid, and damages the articular cartilage, leading to pain and stiffness.
Traumatic Arthritis can follow a serious hip injury or fracture. A hip fracture can cause a condition known as avascular necrosis. The articular cartilage becomes damaged and, over time, causes hip pain and stiffness.
Is hip replacement surgery for you?
The decision whether to have hip replacement surgery should be a cooperative one between you, your family, your primary care doctor, and your orthopaedic surgeon. The process of making this decision typically begins with a referral by your doctor to an orthopaedic surgeon for an initial evaluation.
Although many patients who undergo hip replacement surgery are age 60 to 80, orthopaedic surgeons evaluate patients individually. Recommendations for surgery are based on the extent of your pain, disability and general health status, not solely on age.

You may benefit from hip replacement surgery if:
• Hip pain limits your everyday activities such as walking or bending.
• Hip pain continues while resting, either day or night.
• Stiffness in a hip limits your ability to move or lift your leg.
• You have little pain relief from anti-inflammatory drugs or glucosamine sulfate.
• You have harmful or unpleasant side effects from your hip medications.
• Other treatments such as physical therapy or the use of a gait aid such as a cane don't relieve hip pain.
The orthopaedic evaluation
Your orthopaedic surgeon will review the results of your evaluation with you and discuss whether hip replacement surgery is the best method to relieve your pain and improve your mobility. Other treatment options such as medications, physical therapy or other types of surgery also may be considered.
Your orthopaedic surgeon will explain the potential risks and complications of hip replacement surgery, including those related to the surgery itself and those that can occur over time after your surgery. These risks and complications are discussed later in this booklet.
• A medical history, in which your orthopaedic surgeon gathers information about your general health and asks questions about the extent of your hip pain and how it affects your ability to perform every day activities.
• A physical examination to assess your hip's mobility, strength and alignment.
• X-rays to determine the extent of damage or deformity in your hip.
• Occasionally, blood tests or other tests such as an Magnetic Resonance Imaging (MRI) or a bone scan may be needed to determine the condition of the bone and soft tissues of your hip.
What to expect from hip replacement surgery
An important factor in deciding whether to have hip replacement surgery is understanding what the procedure can and can't do.
Most people who undergo hip replacement surgery experience a dramatic reduction of hip pain and a significant improvement in their ability to perform the common activities of daily living. However, hip replacement surgery will not enable you to do more than you could before your hip problem developed.
Following surgery, you will be advised to avoid certain activities, including jogging and high-impact sports, for the rest of your life. You may be asked to avoid specific positions of the joint that could lead to dislocation.
Even with normal use and activities, an artificial joint (prosthesis) develops some wear over time. If you participate in high-impact activities or are overweight, this wear may accelerate and cause the prosthesis to loosen and become painful.
Preparing for surgery
Medical Evaluation. If you decide to have hip replacement surgery, you may be asked to have a complete physical by your primary care doctor before your surgery. This is needed to assess your health and find conditions that could interfere with your surgery or recovery.
Tests. Several tests such as blood samples, a cardiogram, chest X-rays and urine samples may be needed to help plan your surgery.
Preparing Your Skin. Your skin should not have any infections or irritations before surgery. If either is present, contact your orthopaedic surgeon for a program to improve your skin before your surgery.
Blood Donations. You may be advised to donate your own blood prior to surgery. It will be stored in case you need blood after surgery.
Medications. Tell your orthopaedic surgeon about the medications you are taking. Your orthopaedist or your primary care doctor will advise you which medications you should stop or can continue taking before surgery.
Weight Loss. If you are overweight, your doctor may ask you to lose some weight before surgery to minimize the stress on your new hip, and possibly decrease the risks of surgery
Dental Evaluation. Although infections after hip replacement are not common, an infection can occur if bacteria enter your bloodstream. Because bacteria can enter the bloodstream during dental procedures, you should consider getting treatment for significant dental diseases (including tooth extractions and periodontal work) before your hip replacement surgery. Routine cleaning of your teeth should be delayed for several weeks after surgery.
Urinary Evaluation. Individuals with a history of recent or frequent urinary infections and older men with prostate disease should consider a urological evaluation before surgery.
Social Planning. Although you will be able to walk with crutches or a walker soon after surgery, you will need some help for several weeks with such tasks as cooking, shopping, bathing and laundry. If you live alone, your surgeon's office, a social worker, or a discharge planner at the hospital can help you make advance arrangements to have someone assist you at your home. A short stay in an extended care facility during your recovery after surgery also may be arranged.
Home planning
Here are some items and home modifications that will make your return home easier during your recovery.
• Securely fastened safety bars or handrails in your shower or bath
• Secure handrails along all stairways
• A stable chair for your early recovery with a firm seat cushion that allows your knees to remain lower than your hips, a firm back and two arms
• A raised toilet seat
• A stable shower bench or chair for bathing
• A long-handled sponge and shower hose
• A dressing stick, a sock aid and a long-handled shoe horn for putting on and taking off shoes and socks without excessively bending your new hip
• A reacher that will allow you to grab objects without excessive bending of your hips
• Firm pillows to sit on that keep your knees lower than your hips for your chairs, sofas and car
• Removal of all loose carpets and electrical cords from the areas where you walk in your home
Your surgery
You will most likely be admitted to the hospital on the day of your surgery. Prior to admission, a member of the anesthesia team will evaluate you. The most common types of anesthesia for hip replacement surgery are general anesthesia (which puts you to sleep throughout the procedure and uses a machine to help you breath) or spinal anesthesia (which allows you to breath on your own but anesthetizes your body from the waist down). The anesthesia team will discuss these choices with you and help you decide which type of anesthesia is best for you.
Surgical procedure
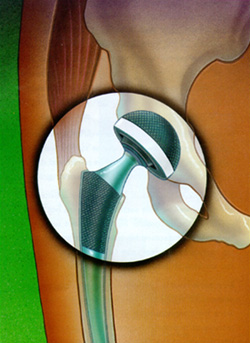
The surgical procedure takes a few hours. Your orthopaedic surgeon will remove the damaged cartilage and bone, then position new metal, plastic or ceramic joint surfaces to restore the alignment and function of your hip.
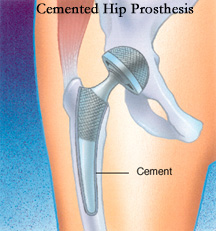
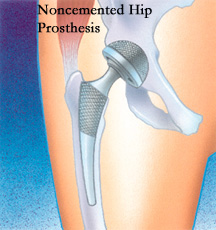
Many different types of designs and materials are currently used in artificial hip joints. All of them consist of two basic components: the ball component (made of a highly polished strong metal or ceramic material) and the socket component (a durable cup of plastic, ceramic or metal, which may have an outer metal shell).
Special surgical cement may be used to fill the gap between the prosthesis and remaining natural bone to secure the artificial joint.
A noncemented prosthesis has also been developed which is used most often in younger, more active patients with strong bone. The prosthesis may be coated with textured metal or a special bone-like substance, which allows bone to grow into the prosthesis.
A combination of a cemented ball and a noncemented socket may be used.
Your orthopaedic surgeon will choose the type of prosthesis that best meets your needs.
After surgery, you will be moved to the recovery room where you will remain for one to two hours while your recovery from anesthesia is monitored. After you awaken fully, you will be taken to your hospital room.
A special note about minimally invasive total hip replacement
Over the past several years, orthopaedic surgeons have been developing new techniques, known as minimally invasive hip replacement surgery, for inserting total hip replacements through smaller incisions. It is hoped, but not yet proven, that this may allow for quicker, less painful recovery and more rapid return to normal activities. Minimally invasive and small incision total hip replacement surgery is a rapidly evolving area. While certain techniques have proven to be safe, others may be associated with an increased risk of complications such as nerve and artery injuries, wound healing problems, infection, fracture of the femur and malposition of the implants, which can contribute to premature wear, dislocation and loosening of your hip replacement. Patients who have marked deformity of the joint, those who are heavy or muscular, and those who have other health problems, which can contribute to wound healing problems, appear to be at higher risk of problems. Your orthopaedic surgeon can talk to you about his or her experience with minimally invasive hip replacement surgery and the possible risks and benefits of minimally invasive hip replacement surgery. The AAOS and the American Association of Hip and Knee Surgeons have developed information for patients about minimally invasive hip replacement surgery.
Your stay in the hospital
You will usually stay in the hospital for a few days. After surgery, you will feel pain in your hip. Pain medication will be given to make you as comfortable as possible.
To avoid lung congestion after surgery, you will be asked to breathe deeply and cough frequently.
To protect your hip during early recovery, a positioning splint, such as a V-shaped pillow placed between your legs, may be used.
Walking and light activity are important to your recovery and will begin the day of or the day after your surgery. Most hip replacement patients begin standing and walking with the help of a walking support and a physical therapist the day after surgery. The physical therapist will teach you specific exercises to strengthen your hip and restore movement for walking and other normal daily activities.
Possible complications after surgery
The complication rate following hip replacement surgery is low. Serious complications, such as joint infection, occur in less than 2 percent of patients. Major medical complications, such as heart attack or stroke, occur even less frequently. However, chronic illnesses may increase the potential for complications. Although uncommon, when these complications occur they can prolong or limit your full recovery.
Blood clots in the leg veins or pelvis are the most common complication of hip replacement surgery. Your orthopaedic surgeon may prescribe one or more measures to prevent blood clots from forming in your leg veins or becoming symptomatic. These measure may include special support hose, inflatable leg coverings, ankle pump exercises and blood thinners.
Leg-length inequality may occur or may become or seem worse after hip replacement. Your orthopaedic surgeon will take this into account, in addition to other issues, including the stability and biomechanics of the hip. Some patients may feel more comfortable with a shoe lift after surgery.
Other complications such as dislocation, nerve and blood vessel injury, bleeding, fracture and stiffness can occur. In a small number of patients, some pain can continue, or new pain can occur after surgery.
Over years, the hip prosthesis may wear out or loosen. This problem will likely be less common with newer materials and techniques. When the prosthesis wears, bone loss may occur because of the small particles produced at the wearing surface. This process is called osteolysis.
Your recovery at home
The success of your surgery will depend in large measure on how well you follow your orthopaedic surgeon's instructions regarding home care during the first few weeks after surgery
Wound Care. You will have stitches or staples running along your wound or a suture beneath your skin. The stitches or staples will be removed about two weeks after surgery.
Avoid getting the wound wet until it has thoroughly sealed and dried. A bandage may be placed over the wound to prevent irritation from clothing or support stockings.
Diet. Some loss of appetite is common for several weeks after surgery. A balanced diet, often with an iron supplement, is important to promote proper tissue healing and restore muscle strength. Be sure to drink plenty of fluids.
Activity. Exercise is a critical component of home care, particularly during the first few weeks after surgery. You should be able to resume most normal light activities of daily living within three to six weeks following surgery. Some discomfort with activity and at night is common for several weeks.
Your activity program should include:
• A graduated walking program, initially in your home and later outside
• Walking program to slowly increase your mobility and endurance
• Resuming other normal household activities
• Resuming sitting, standing, walking up and down stairs
• Specific exercises several times a day to restore movement
• Specific exercises several times a day to strength your hip joint
• May wish to have a physical therapist help you at home
Avoiding problems after surgery
Blood Clot Prevention. Follow your orthopaedic surgeon's instructions carefully to minimize the potential risk of blood clots, which can occur during the first several weeks of your recovery.
Warning signs of possible blood clots include:
• Pain in your calf and leg, unrelated to your incision
• Tenderness or redness of your calf
• Swelling of your thigh, calf, ankle or foot
Warning signs that a blood clot has traveled to your lung include:
• Shortness of breath
• Chest pain, particularly with breathing
Notify your doctor immediately if you develop any of these signs.
Preventing infection
The most common causes of infection following hip replacement surgery are from bacteria that enter the bloodstream during dental procedures, urinary tract infections, or skin infections. These bacteria can lodge around your prosthesis.
Following your surgery, you may need to take antibiotics prior to dental work, including dental cleanings, or any surgical procedure that could allow bacteria to enter your bloodstream. For many patients with a normal immune system the AAOS and ADA recommend dental prophylaxis for two years after a primary total joint surgery. A complete discussion of this topic is available on the AAOS patient education Web site, Your Orthopaedic Connection.
Warning signs of a possible hip replacement infection are:
• Persistent fever (higher than 100 degrees orally)
• Shaking chills
• Increasing redness, tenderness or swelling of the hip wound
• Drainage from the hip wound
• Increasing hip pain with both activity and rest
Notify your doctor immediately if you develop any of these signs.
Avoiding falls
A fall during the first few weeks after surgery can damage your new hip and may result in a need for more surgery. Stairs are a particular hazard until your hip is strong and mobile. You should use a cane, crutches, a walker or handrails, or have someone help you until you improve your balance, flexibility and strength.
Your surgeon and physical therapist will help you decide what assistive aides will be required following surgery, and when those aides can safely be discontinued.
Other precautions
To assure proper recovery and prevent dislocation of the prosthesis, you must take special precautions. Do not cross your legs. Do not bend your hips more than a right angle (90 degrees). Do not turn your feet excessively inward or outward. Use a pillow between your legs at night when sleeping until you are advised by your orthopaedic surgeon that you can remove it. Your surgeon and physical therapist will give you more instructions prior to your discharge from the hospital.
How your new hip is different
You may feel some numbness in the skin around your incision. You also may feel some stiffness, particularly with excessive bending. These differences often diminish with time and most patients find these are minor compared to the pain and limited function they experienced prior to surgery.
Your new hip may activate metal detectors required for security in airports and some buildings. Tell the security agent about your hip replacement if the alarm is activated. You may ask your orthopaedic surgeon for a card confirming that you have an artificial hip.
After surgery, make sure you also do the following:
• Participate in a regular light exercise program to maintain proper strength and mobility of your new hip.
• Take special precautions to avoid falls and injuries. Individuals who have undergone hip replacement surgery and suffer a fracture may require more surgery.
• Notify your dentist that you have had a hip replacement. You will need to take antibiotics before any dental procedure for a minimum of two years after your surgery and possibly longer, depending on your past health history. Guidelines for the use of antibiotics for your surgeon and dentist are available from the AAOS and the American Dental Association.
• See your orthopaedic surgeon periodically for routine follow-up examinations and X-rays, even if your hip replacement seems to be doing fine.
Your orthopaedic surgeon is a medical doctor with extensive training in the diagnosis and nonsurgical and surgical treatment of the musculoskeletal system, including bones, joints, ligaments, tendons, muscles, and nerves.
Herniated Disc Surgery
Herniated Disk
Description
You've probably heard people say they have a "slipped" or "ruptured" disk in their neck or lower back. What they're actually describing is a herniated disk, a common source of neck, or lower back and arm or leg pain.
Disks are soft, rubbery pads found between the hard bones (vertebrae) that make up the spinal column. In the middle of the spinal column is the spinal canal-a hollow space that contains the spinal cord and other nerve roots. The disks between the vertebrae allow the back to flex or bend. Disks also act as shock absorbers.
Disks in the lumbar spine (low back) are composed of a thick outer ring of cartilage (annulus) and an inner gel-like substance (nucleus). In the cervical spine (neck), the disks are similar but smaller in size. A helpful comparison is a jelly donut: its thick outer portion represents the annulus, while the jelly is similar to the nucleus.
A disk herniates or ruptures when part of the center nucleus pushes through the outer edge of the disk. To continue with the donut analogy, the jelly pushes backwards toward the spinal canal. This puts pressure on the nerves. Spinal nerves are very sensitive to even slight amounts of pressure. Pain, numbness or weakness may occur in one or both legs.
Risk Factors/Prevention
In children and young adults, disks have high water content. As people age, the water content in the disks decreases. They become less flexible. The disks begin to shrink. The spaces between the vertebrae get narrower. The disk itself becomes less flexible. Conditions that can weaken the disk include:
• Improper lifting
• Smoking
• Excessive body weight that places added stress on the disks (in the lower back)
• Sudden pressure (which may be slight)
• Repetitive strenuous activities
Symptoms
Lower Back: Low back pain affects four out of five people. Pain alone isn't enough to recognize a herniated disk. See your doctor if back pain results from a fall or a blow to your back. The most common symptom of a herniated disk is sciatica-a sharp, often shooting pain that extends from the buttocks down the back of one leg. It is caused by pressure on the spinal nerve. Other symptoms include:
• Weakness in one leg
• Tingling (a "pins-and-needles" sensation) or numbness in one leg or buttock
• Loss of bladder or bowel control (If you also have significant weakness in both legs, you could have a serious problem. Seek immediate attention.)
• A burning pain centered in the neck
Neck: Like pain in the lower back, neck pain is also common. When pressure is placed on a nerve in the neck, it causes pain in the muscles between your neck and shoulder (trapezial muscles). The pain may shoot down the arm. Sometimes the pain causes headaches in the back of the head. Other symptoms include:
• Weakness in one arm
• Tingling (a "pins-and-needles" sensation) or numbness in one arm
• Loss of bladder or bowel control (If you also have significant weakness in both arms or legs, you could have a serious problem. Seek immediate attention.)
• Burning pain in the shoulders, neck or arm
Diagnosis
To diagnose a herniated disk, give the doctor your complete medical history. Tell him or her if you have neck/back pain with gradually increasing arm/leg pain. Tell the doctor if you were injured. The doctor will physically examine you. This can determine which nerve roots are affected (and how seriously). A simple X-ray may show evidence of disk or degenerative spine changes.
MRI (magnetic resonance imaging) or CT (computed tomography) scans (imaging tests to confirm which disk is injured) or an EMG (a test that measures nerve impulses to the muscles) may be recommended if pain continues.
Treatment Options
Conservative treatment is effective in treating symptoms of herniated disks in more than 90 percent of patients. Most neck or back pain will resolve gradually with simple measures.
• Bed rest and over-the-counter pain relievers may be all that's needed.
• Muscle relaxers, analgesic and anti-inflammatory medications are also helpful.
• You can also apply cold compresses or ice for no more than 20 minutes at a time, several times a day.
• After any spasms settle, you can switch to gentle heat applications.
Any physical activity should be slow and controlled, especially bending forward and lifting. This can help ensure that symptoms do not return. Take short walks and avoid sitting for long periods. For the lower back, exercises may also be helpful in strengthening back and abdominal muscles. For the neck, exercises or traction may also be helpful. It's essential that you learn how to properly stand, sit and lift. This can help you avoid future episodes of pain.
Treatment Options: Surgical
If conservative treatment fails, epidural injections of a cortisone-like drug may lessen nerve irritation and allow better participation in physical therapy. These shots are given on an outpatient basis over a period of weeks.
Surgery may be required if a disk fragment lodges in the spinal canal and presses on a nerve, causing significant loss of function. Surgical options in the lower back include microdiskectomy or laminectomy depending on the size and position of the disk herniation. In the neck, an anterior cervical discectomy and fusion is usually recommended. This involves removing the entire disk to take the pressure off the spinal cord and nerve roots. Bone is placed in the disc space and a metal plate may be used to stabilize the spine. On occasion, a smaller surgery may be performed on the back of the neck that does not require fusing the bones together. Each of these surgeries is performed under general anesthesia. It may be performed as an outpatient or require an overnight hospital stay. You should be able to return to work in two to six weeks.
Lumbar Spinal Stenosis. Laminectomy
Lumbar Spinal Stenosis
Description
The lumbar spine (lower back) provides a foundation to carry the weight of the upper body. It also houses the nerves that control the lower body. With aging, the discs in the front of the spine become dehydrated. The joints in the back of the spine become overgrown due to arthritis. These degenerative changes are the result of the normal "wear-and-tear" associated with aging. Over time these changes can also lead to narrowing, or stenosis, of the spinal canal (see Figure 1).
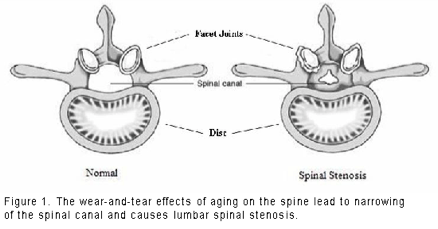
Narrowing of the lumbar spinal canal pinches the nerves that control muscle power and sensation in the legs. Sometimes the pinched nerves become inflamed and cause pain in the buttocks and/or legs. These changes also can diminish the ability of the spine to carry the load of the upper body. They can lead to the forward slippage of one vertebra on another. This slippage, called "degenerative spondylolisthesis," can cause both back and leg pain.
Your orthopaedic surgeon can diagnose lumbar spinal stenosis using a combination of:
• Your symptoms
• Physical examination
• Plain X-rays
• Magnetic resonance imaging (MRI)
X-rays can show the presence of arthritis and slippage of the vertebrae. An MRI is used to determine whether nerves are being pinched. For people who cannot get an MRI (for example, people with pacemakers), a special test called a computed tomography (CT) myelogram may be necessary. This test requires the injection of a dye into the spine to make the nerves visible.
Risk Factors/Prevention
Lumbar spinal stenosis is usually caused by the wear-and-tear changes of aging. It usually affects middle-aged and older adults. People who are born with narrower spinal canals are more likely to develop this problem.
The best way to avoid the symptoms of lumbar spinal stenosis is to stay as physically fit as possible. Regular exercise can improve endurance and keep the muscles that support the spine strong. Avoiding weight gain can decrease the load that the lumbar spine has to carry. Patients should also avoid cigarette smoking. Both the smoke and the nicotine cause the spine to degenerate faster than normal.
Symptoms
Typically patients with lumbar spinal stenosis have a long history of pain in the back, buttocks or legs that gradually becomes worse. The symptoms are usually worsened by standing or walking upright. This results in an achy pain, tightness, heaviness and a sense of weakness in the buttocks and/or legs. These symptoms are generally relieved by sitting down or leaning forward. Although patients are unable to walk for very long, they may be able to ride an exercise bicycle for much longer. Some patients also find that it is easier to walk while leaning forward on a shopping cart. This position tends to create more space in the spinal canal. Leaning onto the handlebars of a bicycle creates the same effect. This relieves some of the pressure on the nerves.
Treatment Options
Non-surgical options to relieve the symptoms of lumbar spinal stenosis include:
A program of physical therapy with activity modifications. A program of gentle physical therapy may help. This program usually includes:
• Aerobic conditioning--the exercise bicycle is a good way for patients with lumbar spinal stenosis to workout without pain. Pool exercises can help people who cannot do aerobic exercises on land.
• Strengthening exercises
• Flexibility
• Other modalities
Anti-inflammatory medications--such as ibuprofen and naproxen--may be prescribed. These medications decrease pain and inflammation. Although they can be helpful, these medicines can have serious side effects. Prolonged use can lead to gastrointestinal ulcers, bleeding and kidney problems. Some of them may also increase the risk of heart attacks or strokes.
Epidural steroid injections. These injections deliver anti-inflammatory medication directly into the spinal canal and to the area of the inflammation. These injections are more effective than the medications taken by mouth. They may also have fewer side effects.
These injections deliver steroid medication straight to the nerve roots that are being pinched. Such steroid injections can give relief for weeks to months. They allow the patient to participate in more aggressive rehabilitation. In some cases, they may enable a patient to postpone or avoid surgical treatment altogether.
Bracing is generally not recommended for long-term use. If used for too long, bracing can lead to deconditioning of the muscles that support the back. Acupuncture or chiropractic manipulation can also be attempted.
All these nonsurgical treatments are aimed at decreasing inflammation. They also decrease the symptoms that patients experience. However, these treatments do not improve the narrowing of the spinal canal.
Treatment Options: Surgical
Most people with lumbar spinal stenosis do not require surgery. However, if patients are experiencing severe pain that limits their activities of daily living and their ability to have a good quality of life, surgery may be recommended. In general, surgery is only considered as a last resort if all attempts at non-surgical therapies are unsuccessful and if the overall potential benefits of surgery are greater than the potential risks. Surgery may be recommended on an urgent basis if a patient has severe weakness or loss of bowel and bladder control.
The surgical procedure for lumbar spinal stenosis involves removing the bone and soft tissue that are pinching the nerves. This is called "decompression" or "laminectomy." Some patients require only a decompression. However, patients with slippage of the spine or a curvature of the spine may require a stabilization procedure called fusion. In this procedure, two or more vertebrae are fused together using a bone graft harvested from the hip.
Fusion eliminates motion and prevents the slippage or curvature from worsening after surgery, which would cause more back and/or leg pain. Your surgeon may use screws and rods to hold the spine in place while the body heals the bone together (see Figure 2). Using screws and rods increases the rate of fusion and enables the patient to get out of the postoperative brace sooner. Overall the results of surgery are good to excellent in about 80 percent of patients. Patients tend to see better improvement of leg pain than back pain. Most patients are able to resume a normal lifestyle after a period of recovery from surgery.
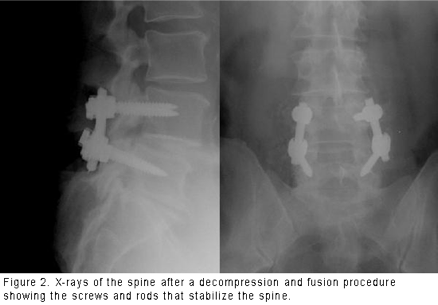
There are some risks to surgery, including:
• Bleeding
• Infection
• Blood clots
• Reaction to anesthesia
• Tear of the sac covering the nerves (dural tear)
• Failure to relieve symptoms
• Return of symptoms after some time
• Failure of the bone fusion to heal
• Failure of screws or rods
• Need for further surgery
• Injury to the nerves
The risks of surgery depend on the patient and the exact procedure being performed. Elderly patients have higher rates of complications from surgery. So do overweight patients, diabetics, smokers and patients with multiple medical problems.
After surgery, patients may be hospitalized for several days, depending on the patient and the procedure performed. Relatively healthy patients who only have a decompression procedure may be able to return home the same day. They usually return to normal activities after a few weeks.
Patients who have a fusion procedure are hospitalized for several days. They usually receive an outpatient physical therapy program. A lumbar corset or brace may also be prescribed after surgery. They return to normal activities after two to three months. Older patients who need more physical therapy may be transferred from the hospital to a rehabilitation facility.
Research on the Horizon/What's New?
There are two areas of research that may change the way patients with spinal stenosis are treated. First, surgeons are developing ways to perform decompression procedures through smaller incisions. These techniques may cause less pain after the operation. They may allow quicker return to normal activities. Researchers are studying whether these new techniques are as effective and safe as the traditional procedures.
Arthroscopic Rotator Cuff Repair
Rotator Cuff Tears
Description
Rotator cuff tear is a common cause of pain and disability in the adult population. The rotator cuff is made up of four muscles and their tendons. These combine to form a "cuff" over the upper end of the arm (head of the humerus). The four muscles - supraspinatus, infraspinatus, subscapularis, and teres minor - originate from the "wing bone"(scapula), and together form a single tendon unit. This inserts on the greater tuberosity of the humerus. The rotator cuff helps to lift and rotate the arm and to stabilize the ball of the shoulder within the joint.
Most tears occur in the supraspinatus but other parts of the tendon may be involved.
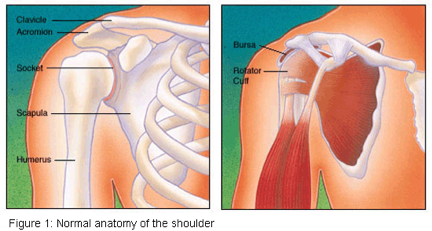
Risk Factors/Prevention
Rotator cuff tear is most common in people who are over the age of 40. It may occur in younger patients following acute trauma or repetitive overhead work or sports activity. Common examples are:
• Workers who do overhead activities such as painting, stocking shelves or construction
• Athletes such as swimmers, pitchers and tennis players
A cuff tear may also happen with another injury to the shoulder, such as a fracture or dislocation.
Symptoms
Symptoms of a rotator cuff tear may develop acutely or have a more gradual onset. Acute pain usually follows trauma such as a lifting injury or a fall on the affected arm. More commonly, the onset is gradual and may be caused by repetitive overhead activity or by wear and degeneration of the tendon. You may feel pain in the front of your shoulder that radiates down the side of your arm. At first the pain may be mild and only present with overhead activities such as reaching or lifting. It may be relieved by over-the-counter medication such as aspirin or ibuprofen. Over time the pain may become noticeable at rest or with no activity at all. There may be pain when you lie on the affected side and at night. Other symptoms may include stiffness and loss of motion. You may have difficulty using your arm to reach overhead to comb your hair or difficulty placing your arm behind your back to fasten a button.
When the tear occurs with an injury, there may be sudden acute pain, a snapping sensation and an immediate weakness of the arm.

Diagnosis
Diagnosis of a rotator cuff tear is based on your symptoms, your doctor's examination, X-rays, and imaging studies such as MRI (magnetic resonance imaging). Your doctor will examine your shoulder to see if it is tender in any area or if there is a deformity. He or she will measure the range of motion of your shoulder in several different directions and test the strength of your arm. The doctor will also check for instability and problems with the AC (acromioclavicular) joint.
The doctor may also examine your neck to make sure that your pain is not coming from a "pinched nerve" in your cervical spine and to rule out other conditions such as osteoarthritis or rheumatoid arthritis.
Some of the signs of a rotator cuff tear include:
• Atrophy or thinning of the muscles about the shoulder
• Pain when you lift your arm
• Pain when you lower your arm from a fully raised position
• Weakness when you lift or rotate your arm
• Crepitus or crackling sensation when you move your shoulder in certain positions
Plain X-rays of a shoulder with a rotator cuff tear are usually normal or show a small spur. For this reason, your doctor may order an additional study such as an ultrasound or MRI. These can better visualize soft tissue structures such as the rotator cuff tendon.
An MRI can sometimes distinguish between a full thickness (complete) tear of the tendon and a partial tear. It can show the doctor if the tear is within the tendon itself, or if the tendon is detached from bone.
In some circumstances, an Arthrogram, in which local anaesthetic and dye is injected into the joint, may also be helpful.
Treatment Options
Once a diagnosis of rotator cuff tear has been made, your orthopaedic surgeon will recommend the most effective treatment. In many instances, non-surgical treatment can provide pain relief and can improve the function of your shoulder.
Treatment options may include:
• Rest and limited overhead activity
• Use of a sling
• Anti-inflammatory medication
• Steroid injection
• Strengthening exercise and physical therapy
It may take several weeks or months to restore the strength and mobility to your shoulder.
Treatment Options: Surgical
Your orthopaedic surgeon may recommend surgery if nonoperative treatment does not relieve your symptoms. Surgery may also be considered if the tear is acute and painful, if it is the dominant arm of an active individual or if you need maximum strength in your arm for overhead work or sports.
The type of surgery performed depends on the size, shape and location of the tear. A partial tear may require only a trimming or smoothing procedure called a "debridement." A complete tear within the substance of the tendon is repaired by suturing the two sides of the tendon. If the tendon is torn from its insertion on the greater tuberosity of the humerus, it can be repaired directly to bone.
Many surgical repairs can be done on an outpatient basis.
In the operating room, your surgeon may remove part of the front portion of the scapula, the acromion as part of the procedure. The acromion is thought to cause "impingement" on the tendon. This may lead to a tear. Other conditions such as arthritis of the AC joint or tearing of the biceps tendon may also be addressed.
In general, three approaches are available for surgical repair. These include :
Arthroscopic Repair
A fiberoptic scope and small instruments are inserted through small puncture wounds instead of an open incision. The scope is connected to a television monitor and the surgeon can perform the repair under video control.
Mini-Open Repair
Newer techniques and instruments allow surgeons to perform a complete rotator cuff repair through a small incision, typically 4 cm to 6 cm.
Open Surgical Repair
A traditional open surgical incision is often required if the tear is large or complex or if additional reconstruction such as a tendon transfer has to be done. In some severe cases, where arthritis has developed, shoulder replacement is an option.
Your surgeon will recommend which technique is best for you.
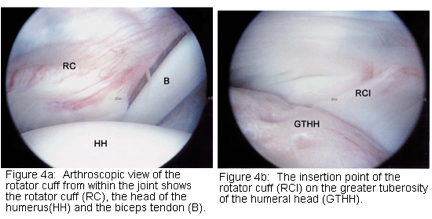
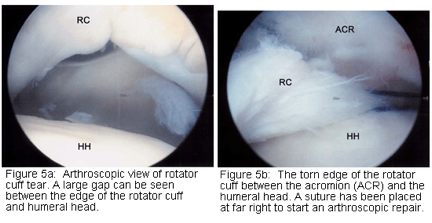
Rehabilitation
After surgery, the arm is immobilized to allow the tear to heal. The length of immobilization depends upon the severity of the tear. You will be given an exercise program to help regain motion and strength in the shoulder. This begins with passive motion. It advances to active and resistive exercises. Your orthopaedic surgeon may recommend that you work with a physical therapist. Complete recovery may take several months.
A strong commitment to rehabilitation is important to achieve a good surgical outcome. The doctor will advise you when it is safe to return to overhead work and sports activity.
Research on the Horizon/What's New?
Future developments in the treatment of rotator cuff disease include newer arthroscopic and mini-open surgical techniques. These allow for smaller, less painful incisions and faster recovery time. Many techniques now use dissolvable anchors. These hold stitches in place or hold stitches down to bone until the repair has healed and then are absorbed by the body. Research is also being done on "orthobiologic" tissue implants. These promote growth of new tissue in the body, and help with the healing process.
Arthroscopic Shoulder Decompression
Shoulder Impingement
Description
Impingement is one of the most common causes of pain in the adult shoulder. It results from pressure on the rotator cuff from part of the shoulder blade (scapula) as the arm is lifted.
The rotator cuff is a tendon linking four muscles - the supraspinatus, the infraspinatus, the subscapularis, and the teres minor. These muscles cover the "ball" of the shoulder (head of the humerus). The muscles work together to lift and rotate the shoulder.
The acromion is the front edge of the shoulder blade. It sits over and in front of the humeral head. As the arm is lifted, the acromion rubs or "impinges" on the surface of the rotator cuff. This causes pain and limits movement.
The pain may be due to a "bursitis" or inflammation of the bursa overlying the rotator cuff or a "tendonitis" of the cuff itself. In some circumstances, a partial tear of the rotator cuff may cause impingement pain.
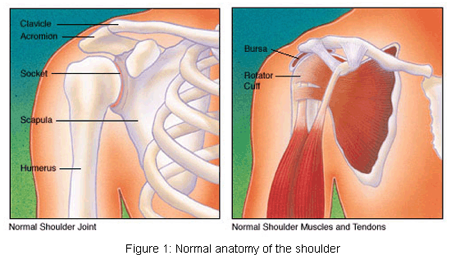
Risk Factors/Prevention
Impingement is common in both young athletes and middle-aged people. Young athletes who use their arms overhead for swimming, baseball and tennis are particularly vulnerable. Those who do repetitive lifting or overhead activities using the arm such as paper hanging, construction or painting are also susceptible. Pain may also develop as the result of minor trauma or spontaneously with no apparent cause.
Symptoms
Beginning symptoms may be mild. Patients frequently do not seek treatment at an early stage.
• You may first be aware of minor pain that's present both with activity and at rest.
• You may have pain radiating from the front of the shoulder to the side of the arm.
• You may note sudden pain with lifting and reaching movement.
• Athletes in overhead sports may have pain when throwing or serving a tennis ball.
Impingement commonly causes local swelling and tenderness in the front of the shoulder. There may be pain and stiffness when you attempt to lift your arm. There may also be pain when you lower the arm from an elevated position.
As the problem progresses, you may have pain at night. You may lose strength and motion. You may have difficulty with activities that place the arm behind the back, such as buttoning or zippering. In advanced cases, loss of motion may progress to a "frozen shoulder." In acute bursitis, the shoulder may be severely tender. All movement may be limited and painful.
Diagnosis
To diagnose shoulder impingement, an orthopaedic surgeon reviews the symptoms and physically examines the shoulder.
He or she may take X-rays. A special X-ray view called an "outlet view" sometimes will show a small bone spur on the front edge of the acromion (see Figures 3a and 3b). The doctor may request further imaging studies, such as an MRI (magnetic resonance imaging). These can show fluid or inflammation in the bursa and rotator cuff. In some cases, partial tearing of the rotator cuff will be identified.
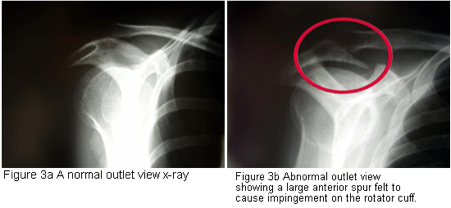
An impingement test, injection of local anesthetic into the bursa, can help to confirm the diagnosis.
Treatment Options
Initial treatment is conservative. The doctor may suggest that you rest and avoid overhead activities. He or she might prescribe a course of oral non-steroidal anti-inflammatory medication. Stretching exercises to improve range of motion in a stiff shoulder will also help.
Many patients benefit from injection of local anesthetic and a cortisone preparation to the affected area. The doctor might also recommend a program of supervised physical therapy. Treatment may take several weeks to months. Many patients experience a gradual improvement and return to function.
Treatment Options: Surgical
When conservative treatment does not relieve pain, the doctor may recommend surgery. The goal of surgery is to remove the impingement and create more space for the rotator cuff. This allows the humeral head to move freely in the subacromial space and to lift the arm without pain. The most common surgical treatment is subacromial decompression or anterior acromioplasty. This may be performed by either arthroscopic or open techniques:
Arthroscopic technique: In an arthroscopic procedure, two or three small puncture wounds are made. The joint is examined through a fiberoptic scope connected to a television camera. Small instruments are used to remove bone and soft tissue.
Open technique: Open surgery requires placement of a small incision in the front of the shoulder. This allows for direct visualization of the acromion and rotator cuff.
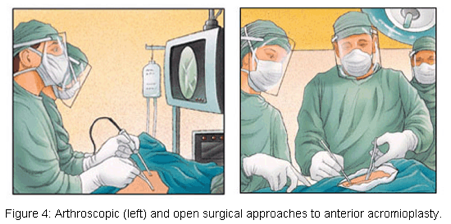
In most cases the front (anterior) edge of the acromion is removed along with some of the bursal tissue. The surgeon may also treat other conditions present in the shoulder at the time of impingement surgery. These can include acromioclavicular arthritis, biceps tendonitis or a partial rotator cuff tear.
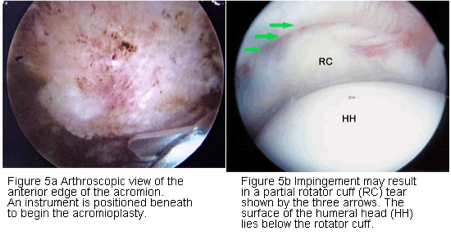
Rehabilitation
After surgery, the arm may be placed in a sling for a short period of time. This allows for early healing. As soon as you are comfortable, you may remove the sling and begin exercise and use of the arm. The surgeon will provide a rehabilitation program based on your needs and the findings at surgery. This will include exercises to regain range of motion of the shoulder and strength of the arm. It may take two to four months to achieve complete relief of pain.
Knee Implants
More joint replacement surgeries (arthroplasties) are performed on the knee than on any other joint. In a total knee arthroplasty (TKA), the diseased cartilage surfaces of the thighbone (femur), the shinbone (tibia) and the kneecap (patella) are replaced by prostheses made of metal alloys, high-grade plastics and polymeric materials. Most of the other structures of the knee, such as the connecting ligaments, remain intact.
Knee replacement surgery is generally recommended for patients with severe knee pain and disability caused by damage to cartilage from rheumatoid arthritis, osteoarthritis or trauma. It is highly successful in relieving pain and restoring joint function.
Implant Design
For simplicity, the knee is considered a hinge joint because of its ability to bend and straighten like a hinged door. In reality, the knee is much more complex because the surfaces actually roll and glide as the knee bends. The first implant designs used the hinge concept and literally included a connecting hinge between the components. Newer implant designs, recognizing the complexity of the joint, attempt to replicate the more complicated motions and to take advantage of the posterior cruciate ligament (PCL) and collateral ligaments for support.
Up to three bone surfaces may be replaced during a TKA: the lower ends (condyles) of the thighbone, the top surface of the shinbone and the back surface of the kneecap. Components are designed so that metal always articulates against plastic, which provides smooth movement and results in minimal wear.
1. Femoral component: The metal femoral component curves around the end of the thighbone and has an interior groove so the kneecap can move up and down smoothly against the bone as the knee bends and straightens. Usually, one large piece is used to resurface the end of the bone. If only one side of the thighbone is damaged, a smaller piece may be used (unicompartmental knee replacement) to resurface just that part of the bone. Some designs (posterior stabilized designs) have an internal post with a circular-shaped device (cam) that works with a corresponding tibial component to help prevent the thighbone from sliding forward too far on the shinbone when you bend the knee.
2. Tibial component: The tibial component is a flat metal platform with a polyethylene cushion. The cushion may be part of the platform (fixed) or separate (mobile) with either a flat surface (PCL-retaining) or a raised, sloping surface (PCL-substituting).
3. Patellar component: The patellar component is a dome-shaped piece of polyethylene that duplicates the shape of the kneecap anchored to a flat metal plate.
There are more than 150 knee replacement designs on the market today. Several manufacturers make knee implants. The brand and design used by your doctor or hospital depends on many factors, including your needs (based on your age, weight, activity level and health), the doctor's experience and familiarity with the device, and the cost and performance record of the implant. You may wish to discuss these issues with your doctor.
Implant Construction
The metal parts of the implant are made of titanium- or cobalt/chromium-based alloys. The plastic parts are made of ultrahigh-density polyethylene. All together, the components weigh between 15 and 20 ounces, depending on the size selected. The construction materials used must meet several criteria:
• They must be biocompatible; that is, they can function in the body without creating either a local or a systemic rejection response.
• Their mechanical properties must be able to duplicate the structures they are intended to replace; for example, they are strong enough to take weightbearing loads, flexible enough to bear stress without breaking and able to move smoothly against each other as required.
• They must be able to retain their strength and shape for a long time. The chance of a knee replacement lasting 15 to 20 years is about 95 percent.
To date, man-made joints have not solved the problem of wear. Every time bone rubs against bone, or metal rubs against plastic, the friction creates microscopic particulate debris. Just as wear in the natural joint contributed to the need for a replacement joint, wear in the prostheses may eventually require a second (revision) surgery.
Implant Insertion
During a TKA, the knee is in a bent position so that all the surfaces to be replaced can be exposed. The usual approach is lengthwise through the front of the knee, just to the inside of the kneecap, although some surgeons will approach the joint from the outer side, just above the kneecap. The incision is 6" to 12" long. The large quadriceps muscle and the kneecap are moved to the side to reveal the bone surfaces.
After taking several measurements to ensure that the new implant will fit properly, the surgeon begins to smooth the rough edges of the bones. Depending on the type of implant used, the surgeon may begin with either the thighbone or the shinbone.
Special jigs are used to accurately trim the damaged surfaces at the end of the thighbone. The devices shape the end of the thighbone so it configures to the inside of the prosthesis. The shinbone is cut flat across the bone and a portion of the bone's center is drilled out. The surgeon removes just enough of the bone so that when the prosthesis is inserted, it recreates the joint line at the same level as prior to surgery. If any ligaments around the knee have contracted due to pain and deformity before the surgery, the surgeon carefully releases them so that they function as close to the normal state as possible.
The prostheses are inserted, tested and balanced. The surgeon wants to be sure that the joint line is in the right place and the kneecap is accurately aligned for proper joint movement. If it is necessary to resurface the kneecap, the surgeon will apply a shaped piece of polyethylene that maintains the original width of the kneecap.
The knee replacement may be "cemented," "cementless" or "hybrid," depending on the type of fixation used to hold the implant in place. Although there are certain general guidelines, each case is individual and your surgeon will evaluate your situation carefully before making any decisions. Do not hesitate to ask what type of fixation will be used in your situation and why that choice is appropriate for you.
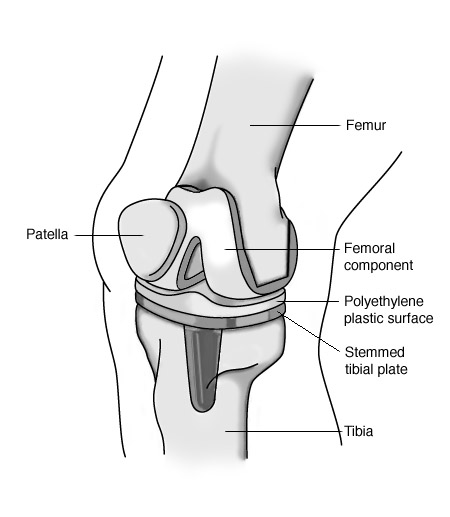
Anesthesia for Hip & Knee Surgery
At some point before your joint replacement surgery, your doctor will raise the issue of anesthesia. Many people will jokingly say, "Just put me out, Doc, and wake me when it's over." But the selection of anesthesia is a major decision that could have a significant impact on your recovery. It deserves careful consideration and discussion with your surgeon and your anesthesiologist.
Several factors must be considered when selecting an anesthesia, including:
• Your past experiences and preferences-Have you ever had anesthesia before? What kind? Did you have a reaction to the anesthesia? What happened? How do other members of your family react to anesthesia?
• Your current health and physical condition-Do you smoke? Are you overweight? Do you drink or use "recreational" drugs? Are you being treated for any condition other than your joint replacement?
• Your reactions to medications-Do you have any allergies? Have you ever experienced bad side effects from a drug? Which drug? What kind of side effects? What medications, nutritional supplements, vitamins or herbal remedies are you currently taking?
• The risks involved-Risks vary, depending on your health and selection of anesthesia, but may include breathing difficulties, blood loss, and allergic reactions. Your surgeon and anesthesiologist will discuss specific risks with you.
• The skill and preferences of your surgical team
There are three broad categories of anesthesia-general, regional, and local. You are probably familiar with local anesthesia, the kind your dentist uses when repairing your teeth. Local anesthesia numbs only the specific area being treated. Most joint replacement surgeries use either general or regional anesthesia.
General anesthesia
General anesthesia affects your entire body. It acts on the brain and nervous system, leaving you in a deep sleep. Usually, it is given by injection or inhalation. When general anesthesia is used, the anesthesiologist will also place a breathing tube down your throat and administer oxygen to assist your breathing. General anesthesia is commonly used if you are having an extensive surgical procedure that takes a long time. There are several types of general anesthetics; your anesthesiologist will discuss specific selections with you.
As with any anesthesia, there are risks, which may be increased if you already have heart disease or a chronic lung condition. General anesthesia slows both your heartbeat and breathing rates, so your heart, blood pressure, breathing and temperature are constantly monitored during the surgery. It also causes your blood vessels to open wider (dilate), which can result in a heavier loss of blood during the surgery. You may want to consider donating blood in advance of your surgery. The tube inserted down your throat may give you a sore throat and hoarse voice for a few days. Headache, nausea and drowsiness are also common.
Regional anesthesia
Regional anesthesia focuses on numbing a specific area of the body, without affecting your brain or breathing. Because you remain conscious, you will be given sedatives to relax you and put you in a light sleep. The two types of regional anesthesia used most frequently in joint replacement surgery are spinal blocks and epidural blocks. For surgery below the hip, a combination block that targets the lumbar plexus and the sciatic nerve can numb only one leg.
In a spinal block, the anesthesia is injected into the fluid surrounding the spinal cord in the lower part of your back. This produces a rapid numbing effect that can last for hours, depending on the drug used. An epidural block uses a small tube (catheter) inserted in your lower back to deliver large quantities of local anesthetics over a longer time period. The epidural block and the spinal block are administered in very similar in location. However, the epidural catheter is placed slightly closer to the skin and further from the spinal cord than the spinal block injection. There are several advantages to using a regional anesthesia during hip or knee replacement surgery. Studies have shown that there is less blood loss during the surgery, and fewer complications from blood clotting afterwards. Side effects from regional anesthesia include headaches, trouble urinating, and allergic reactions, which could be quite serious.
Pain relief after surgery
The goals of postoperative pain management are to enable you to do the required physical therapy and to minimize pain and stress. If a general or spinal anesthesia was used during your surgery, postoperative pain relief may be delivered intravenously. You will be able to control the flow of medication, within preset limits, as you feel the need for additional relief. This process is often referred to as patient-controlled anesthesia, or PCA.
If an epidural block was used during your surgery, the epidural catheter can be left in place and anesthesia continued afterwards to help control pain. You will also have control over the amount of pain medication you receive, within preset limits. You will be closely monitored to ensure that no complications such as excessive sedation or compartment syndrome, an excessive build-up of pressure within the muscles, develop. Your doctor may also prescribe other pain relievers, such as aspirin or ibuprofen, to help control pain after surgery. However, if you are also taking drugs to help prevent blood clots, your use of these pain relievers or any other medications that could further thin the blood will need to be monitored closely.
The proper use of pain relievers before, during, and after your surgery is an extremely important aspect of your treatment, can encourage healing, and can make your joint replacement a more satisfying experience. Take time to discuss the options with your doctor and to ask questions about things you don't understand.
Activities After a Knee Replacement
If you are a candidate for knee replacement surgery, you probably anticipate that life after the surgery will be much like life before it, only without the pain. In many ways, you are correct. But change doesn't happen overnight and your active participation in the healing process is necessary to ensure a successful outcome.
Although you will be able to resume most activities, you should avoid activities that place excessive stress on the new knee. The following suggestions will help you adapt to your new joint and resume your daily activities safely.
Activities in the hospital
The knee is the largest joint in the body, and replacing it is major surgery. Although you'll probably want to take it easy at first, early mobilization is important. If you had considerable pain in your knee, you probably cut back on your activities before surgery and your leg muscles may be weak. You'll need to build up strength in your quadriceps muscles to develop control of your new joint. Early activity is also important to counteract the effects of the anesthesia and to encourage healing. Your doctor and a physical therapist will give you specific instructions on wound care, pain control, diet and exercise.
Proper pain management is important in your early recovery. Although pain after surgery is quite variable and not entirely predictable, it can be controlled with medication. Initially, you will probably receive pain control medication through an intravenous (IV) connection so that you can regulate the amount of medication you need. Remember that it is easier to prevent pain than to control it. You don't have to worry about becoming dependent on the medication; after a day or two, injections or pills will replace the IV. You will also have to take antibiotics and blood-thinning medication to help prevent blood clots from forming in the veins of your thighs and calves.
You may lose your appetite and feel nauseous or constipated for a couple of days. These are normal reactions. You may be fitted with a urinary catheter during surgery and be given stool softeners or laxatives to ease the constipation caused by the pain medication after surgery. You will be taught to do breathing exercises to prevent congestion from developing in your chest and lungs.
Initially, you will have a bulky dressing around the knee and a drain to remove any fluid build up around the knee. The drain will be removed in a day or two. You may also be wearing elastic hose and, possibly, compression stocking sleeves. These plastic sleeves are connected to a machine that circulates air around your legs to help keep blood flowing normally.
Usually a physical therapist will visit you on the day after your surgery and begin teaching you how to use your new knee. You may be fitted with a continuous passive motion (CPM) machine that will slowly and smoothly straighten and bend your knee. Even as you lie in bed, you can "pedal" your feet and "pump" your ankles on a regular basis to promote blood flow in your legs.
Discharge
Your hospital stay may last from 3 to 7 days, depending on how well you heal after surgery. Before you go home, you will need to meet several goals:
1. Get in and out of bed by yourself
2. Bend your knee approximately 90 degrees, or show good progress in bending your knee
3. Extend (straighten) your knee fully
4. Walk with crutches or a walker on a level surface and to climb up and down 2 or 3 stairs
5. Do the prescribed home exercises
You may experience mild swelling in your leg after you are discharged. Elevating the leg, wearing compression hose and applying an ice pack for 15 to 20 minutes at a time will help reduce the swelling. You may be permitted to take the CPM machine home with you for a few weeks, but this is not a substitute for the prescribed exercises.
You will probably need some help at home for several weeks. If you do not have sufficient help at home, you may be temporarily transferred to a rehabilitation center. The following tips can make your homecoming more comfortable.
• Rearrange furniture so you can maneuver with a walker or crutches. You may temporarily change rooms (make the living room your bedroom, for example) to avoid using the stairs.
• Remove any throw or area rugs that could cause you to slip. Securely fasten electrical cords around the perimeter of the room.
• Install a shower chair, gripping bar and raised toilet in the bathroom.
• Use assistive devices such as a long-handled shoehorn, a long-handled sponge and a grabbing tool or reacher to avoid bending too far over.
Activities at home
General guidelines for wound care include:
• Keep the area clean and dry. A dressing will be applied in the hospital and should be changed as necessary. Ask for instructions on how to change the dressing before you leave the hospital.
• Do not shower or bathe until the sutures or staples are removed, usually a week to 10 days after surgery. Keep the wound clean and dry.
• Notify your doctor if the wound appears red or begins to drain.
• Take your temperature twice daily and notify your doctor if it exceeds 100.5°F.
• Swelling is normal for the first three to six months after surgery. Elevate your leg slightly and apply ice.
• Calf pain, chest pain or shortness of breath are signs of a possible blood clot. Notify your doctor immediately if you notice any of these symptoms.
Medication. Take all medications as directed. You will probably be given a blood thinner to prevent clots from forming in the veins of your calf and thigh, because these clots can be life-threatening. If a blood clot forms and then breaks free, it could travel to your lungs, resulting in a pulmonary embolism, a potentially fatal condition.
Because you have an artificial joint, it is especially important to prevent any bacterial infections from settling in your joint implant. You should get a medical alert card and take antibiotics whenever there is the possibility of a bacterial infection, such as when you have dental work. Be sure to notify your dentist that you have a joint implant and let your doctor know if your dentist schedules an extraction, periodontal work, dental implant, or root canal work.
Diet. By the time you go home from the hospital, you should be eating a normal diet. Your physician may recommend that you take iron and vitamin C supplements. Continue to drink plenty of fluids and avoid excessive intake of vitamin K while you are taking the blood thinner medication. Foods rich in vitamin K include broccoli, cauliflower, Brussels sprouts, liver, green beans, garbanzo beans, lentils, soybeans, soybean oil, spinach, kale, lettuce, turnip greens, cabbage and onions. Try to limit your coffee intake and avoid alcohol. You should continue to watch your weight to avoid putting more stress on the joint.
Resuming normal activities: Once you get home, you should continue to stay active. The key is to remember not to overdo it! While you can expect some good days and some bad days, you should notice a gradual improvement and a gradual increase in your endurance over the next 6 to 12 months. The following guidelines are generally applicable, but the final answer on each of these issues should come from your doctor.
• Physical therapy exercises: Continue to do the exercises prescribed for at least two months after surgery. Riding a stationary bicycle can help maintain muscle tone and keep your knee flexible. Try to achieve the maximum degree of bending and extension possible.
• Driving: If your left knee was replaced and you have an automatic transmission, you may be able to begin driving in a week or so, provided you are no longer taking narcotic pain medication. If your right knee was replaced, avoid driving for 6 to 8 weeks. Remember that your reflexes may not be as sharp as before your surgery.
• Airport metal detectors: The sensitivity of metal detectors varies and it is unlikely that your prosthesis will cause an alarm. You should carry a medic alert card indicating you have an artificial joint, just in case.
• Sexual relations can be safely resumed approximately 4 to 6 weeks after surgery.
• Sleeping positions: You can safely sleep on your back, on either side, or on your stomach.
• Return to work: Depending on the type of activities you perform, it may be 6 to 8 weeks before you return to work.
• Other activities: Walk as much as you like, but remember that walking is no substitute for the exercises your doctor and physical therapist will prescribe. Swimming is also recommended; you can begin as soon as the sutures have been removed and the wound is healed, approximately 6 to 8 weeks after surgery. Acceptable activities include dancing, golfing (with spikeless shoes and a cart), and bicycling (on level surfaces). Avoid activities that put stress on the knee. These activities include: tennis, badminton, contact sports (football, baseball), squash or racquetball, jumping, squats, skiing or jogging. Do not do any heavy lifting (more than 40 pounds) or weight lifting.
Sample Exercises
These exercises will help strengthen the quadriceps muscles on the front of the thigh that stabilize and move the knee.
1. Lie on your back with your arms at your side and your legs straight, together, and flat. Place a rolled towel or small pillow under your ankles to raise your heel slightly. Tighten the muscles on the top of one thigh as you push the back of your knee down toward the floor (bed). Hold for 5 seconds, relax for 5 seconds. Do 10 cycles with each leg.
2. Put a rolled blanket or pillow under your knee so that the knee bends about 30 to 40 degrees. Tighten the muscles on the top of your thigh and straighten the knee by lifting your heel off the floor (bed). Hold 5 seconds, then slowly lower your heel to the floor (bed). Repeat 10 to 20 times.
Meniscal Tear
One of the most commonly injured parts of the knee, the meniscus is a wedge-like rubbery cushion where the major bones of your leg connect. Meniscal cartilage curves like the letter "C" at the inside and outside of each knee. A strong stabilizing tissue, the meniscus helps the knee joint carry weight, glide and turn in many directions. It also keeps your femur (thighbone) and tibia (shinbone) from grinding against each other.
Football players and others in contact sports may tear the meniscus by twisting the knee, pivoting, cutting or decelerating. In athletes, meniscal tears often happen in combination with other injuries such as a torn ACL (anterior cruciate ligament). Older people can injure the meniscus without any trauma as the cartilage weakens and wears thin over time, setting the stage for a degenerative tear.
Signs and symptoms
You might experience a "popping" sensation when you tear the meniscus. Most people can still walk on the injured knee and many athletes keep playing. When symptoms of inflammation set in, your knee feels painful and tight. For several days you have:
• Stiffness and swelling.
• Tenderness in the joint line.
• Collection of fluid ("water on the knee").
Without treatment, a fragment of the meniscus may loosen and drift into the joint, causing it to slip, pop or lock—your knee gets stuck, often at a 45-degree angle, until you manually move or otherwise manipulate it. If you think you have a meniscal tear, see your doctor right away for diagnosis and individualized treatment.
Diagnosis
Tell your doctor exactly what happened and when. He or she may conduct physical testing to evaluate the extent of your meniscal tear. You may need X-rays to rule out osteoarthritis or other possible causes of your knee pain. Sometimes your doctor may use a magnetic resonance imaging scan to get a better look at the soft tissues of your knee joint. Your doctor may also use a miniature telescope (arthroscope) to see into your knee joint, especially if your knee locks.
Menisci tear in a number of different ways:
• Young athletes often get longitudinal or "bucket handle" tears if the femur and tibia trap the meniscus when the knee turns.
• Less commonly, young athletes get a combination of tears called radial or "parrot beak" in which the meniscus splits in two directions due to repetitive stress activities such as running.
• In older people, cartilage degeneration that starts at the inner edge causes a horizontal tear as it works its way back.
Conservative treatment
Initial treatment of a meniscal tear follows the basic RICE formula: rest, ice, compression and elevation, combined with nonsteroidal anti-inflammatory medications for pain. If your knee is stable and does not lock, this conservative treatment may be all you need. Blood vessels feed the outer edges of the meniscus, giving that part the potential to heal on its own. Small tears on the outer edges often heal themselves with rest.
Surgical repair
If your meniscal tear does not heal on its own and your knee becomes painful, stiff or locked, you may need surgical repair. Depending upon the type of tear, whether you also have an injured ACL, your age and other factors, your doctor may use an arthroscope to trim off damaged pieces of cartilage.
A cast or brace immobilizes your knee after surgery. You must complete a course of rehabilitation exercises before gradually resuming your activity.
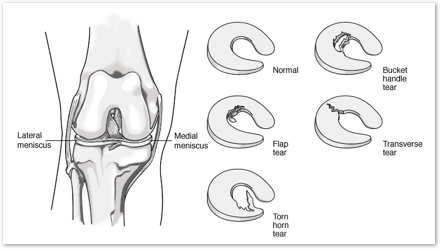
Total Hip Replacement Exercise Guide
Regular exercises to restore your normal hip motion and strength and a gradual return to everyday activities are important for your full recovery. Your orthopaedic surgeon and physical therapist may recommend that you exercise 20 to 30 minutes 2 or 3 times a day during your early recovery. They may suggest some of the following exercises. This can help you better understand your exercise and activity program.
Early Postoperative Exercises
These exercises are important for increasing circulation to your legs and feet to prevent blood clots. They also are important to strengthen muscles and to improve your hip movement. You may begin these exercises in the recovery room shortly after surgery. It may feel uncomfortable at first but these exercises will speed your recovery and reduce your postoperative pain. These exercises should be done as you lie on your back with your legs spread slightly apart.

Ankle Pumps - Slowly push your foot up and down. Do this exercise several
times as often as every 5 or 10 minutes. This exercise can begin immediately
after surgery and continue until you are fully recovered.

Ankle Rotations - Move your ankle inward toward your other foot and then
outward away from your other foot. Repeat 5 times in each direction 3 or 4
times a day.
Repeat the following three exercises 10 times 3 or 4 times a day
Bed-Supported Knee Bends - Slide your heel toward your buttocks, bending
your knee and keeping your heel on the bed. Do not let your knee roll inward.
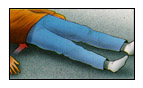
Buttock Contractions - Tighten buttock muscles and hold to
a count of 5.
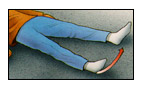
Abduction Exercise - Slide your leg out to the side as far as you
can and then back.
Quad Set - Tighten your thigh muscle. Try to straighten your knee. Hold for
5 to 10 seconds. Repeat this exercise 10 times during a 10-minute period.
Continue until your thigh feels fatigued.
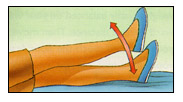
Straight Leg Raises - Tighten your thigh muscle with your knee fully
straightened on the bed. As your thigh muscle tightens, lift your leg several
inches off the bed. Hold for 5 to 10 seconds. Slowly lower. Repeat until your
thigh feels fatigued.
Standing Exercises - Soon after your surgery, you will be out of bed and able to stand. You will require help since you may become dizzy the first several times you stand. As you regain your strength, you will be able to stand independently. While doing these standing exercises, make sure you are holding on to a firm surface such as a bar attached to your bed or a wall.
Repeat the following exercises 10 times 3 or 4 times a day

Standing Knee Raises - Lift your operated leg toward your chest. Do not lift
your knee higher than your waist. Hold for 2 or 3 counts and put your leg down.

Standing Hip Abduction - Be sure your hip, knee and foot are pointing straight
forward. Keep your body straight. With your knee straight, lift your leg out to the
side. Slowly lower your leg so your foot is back on the floor.

Standing Hip Extensions - Lift your operated leg backward slowly. Try to
keep your back straight. Hold for 2 or 3 counts. Return your foot to the floor.
Walking and Early Activity
Soon after surgery, you will begin to walk short distances in your hospital room and perform light everyday activities. This early activity helps your recovery by helping your hip muscles regain strength and movement.
Walking with Walker — Full Weight Bearing - Stand comfortably and erect with your weight evenly balanced on your walker or crutches. Move your walker or crutches forward a short distance. Then move forward, lifting your operated leg so that the heel of your foot will touch the floor first. As you move, your knee and ankle will bend and your entire foot will rest evenly on the floor. As you complete the step allow your toe to lift off the floor. Move the walker again and your knee and hip will again reach forward for your next step. Remember, touch your heel first, then flatten your foot, then lift your toes off the floor. Try to walk as smoothly as you can. Don’t hurry. As your muscle strength and endurance improve, you may spend more time walking. Gradually, you will put more and more weight on your leg.
Walking with Cane or Crutch - A walker is often used for the first several weeks to help your balance and to avoid falls. A cane or a crutch is then used for several more weeks until your full strength and balance skills have returned. Use the cane or crutch in the hand opposite the operated hip. You are ready to use a cane or single crutch when you can stand and balance without your walker, when your weight is placed fully on both feet, and when you are no longer leaning on your hands while using your walker.
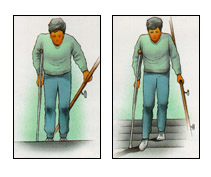
Stair Climbing and Descending - The ability to go up and down stairs requires
both flexibility and strength. At first, you will need a handrail for support and you
will only be able to go one step at a time. Always lead up the stairs with your good
leg and down the stairs with your operated leg. Remember "up with the good" and
"down with the bad." You may want to have someone help you until you have regained
most of your strength and mobility. Stair climbing is an excellent strengthening and
endurance activity. Do not try to climb steps higher than those of the standard height
of seven inches and always use the handrail for balance.
Advanced Exercises and Activities
A full recovery will take many months. The pain from your problem hip before your surgery and the pain and swelling after surgery have weakened your hip muscles. The following exercises and activities will help your hip muscles recover fully. These exercises should be done in 10 repetitions four times a day with one end of the tubing around the ankle of your operated leg and the opposite end of the tubing attached to a stationary object such as a locked door or heavy furniture. Hold on to a chair or bar for balance.
Elastic Tube Exercises

Resistive Hip Flexion - Stand with your feet slightly apart. Bring your
operated leg forward keeping the knee straight. Allow your leg to return
to its previous position.
Resistive Hip Abduction -Stand sideways from the door and extend your
operated leg out to the side. Allow your leg to return to its previous position.

Resistive Hip Extensions - Face the door or heavy object to which the tubing
is attached and pull your leg straight back. Allow your leg to return to its previous
position.
Exercycling - Exercycling is an excellent activity to help you regain muscle strength and hip mobility. Adjust the seat height so that the bottom of your foot just touches the pedal with your knee almost straight. Pedal backwards at first. Pedal forward only after comfortable cycling motion is possible backwards. As you become stronger (at about 4 to 6 weeks) slowly increase the tension on the exercycle. Exercycle forward 10 to 15 minutes twice a day, gradually building up to 20 to 30 minutes 3 to 4 times a week.
Walking - Take a cane with you until you have regained your balance skills. In the beginning, walk 5 or 10 minutes 3 or 4 times a day. As your strength and endurance improves, you can walk for 20 or 30 minutes 2 or 3 times a day. Once you have fully recovered, regular walks, 20 or 30 minutes 3 or 4 times a week, will help maintain your strength.
Minimally Invasive Hip Replacement
Description
Total hip replacement is a common procedure. It involves removing the head of the thighbone (femur). The ball-and-socket mechanism of the hip is replaced with artificial implants.
As the population ages over the next decade, this procedure is expected to become even more common. Patients who undergo hip replacement are typically 60 to 75 years old. More than 90 percent of hip replacements last for 10 years or more. Pain and mobility improve after hip replacement. This allows patients to maintain their independence and quality of life.
Newer techniques and implants have been developed. They make hip replacement a less invasive operation. It takes less time for the patient to recover from surgery. The new implants are engineered to last longer.
Diagnosis
Osteoarthritis of the hip is the most common diagnosis that leads to hip replacement. Osteoarthritis is caused by wear and tear. It affects the cartilage surfaces of the ball-and-socket joint of the hip. The cartilage wears out. Pain and stiffness result. Patients with hip arthritis have difficulty walking, climbing stairs and performing routine daily activities.
Other conditions that can cause destruction of the hip joint include:
• Loss of the blood supply to the head of the thighbone (avascular necrosis)
• Rheumatoid arthritis (an inflammatory autoimmune disease)
• Previous injury or trauma
• Infection
• Developmental abnormalities of the hip
See your doctor to diagnose hip arthritis. Many hip patients have difficulty with walking and day-to-day activities like putting on shoes and socks or climbing stairs. Tell the doctor your symptoms. He or she will perform a physical examination and order X-rays. X-rays typically show loss of the cartilage space in the hip socket. It looks like there is "bone-on-bone". Bone spurs and bone cysts are common. Sometimes, the doctor may recommend additional tests to confirm the diagnosis. These may include MRI (magnetic resonance imaging) or CT (computed tomography) scans.
Risk Factors/Prevention
Hip arthritis may happen if you have a previous injury or mechanical abnormalities related to how the hip developed. Most patients develop arthritis as a result of lifelong wear and tear. Arthritis develops slowly. It takes a period of years. Symptoms increase gradually over time.
Some bone diseases may contribute to the development of hip arthritis. Patients with arthritis may also have brittle bones (osteoporosis). But there is no direct relationship between bone density and the development of arthritis of the hip.
Symptoms
Hip arthritis typically causes pain that is dull and aching. The pain may be constant or it may come and go. You may feel pain in the groin, thigh and buttock. You may also have pain in the knee (referred pain). Walking, especially for longer distances, may cause a limp. Some patients may need a cane, crutch or walker to help them get around. Pain usually starts slowly. It gets worse with time, and higher activity levels.
Climbing stairs can be difficult. Many patients with hip arthritis have to use a stair rail or stop on each step to get up and down. Dressing, tying shoes and clipping toenails can be difficult or impossible. You may have pain when you rest. Pain may interfere with your sleep. Resting and taking anti-inflammatory or pain medication can help.
Treatment Options
The first treatment a doctor may recommend is to take prescription or over-the-counter, anti-inflammatory medications. These include ibuprofen (Motrin®or Advil®acetaminophen (Tylenol®or mild combination narcotics (Tylenol® with codeine). Some nutritional supplements may also provide some relief. These include glucosamine. Short-term physical therapy may help with strength and stiffness.
For more advanced arthritis, you may need to use a cane in the hand opposite the affected hip. This transfers weight away from the affected hip. It can improve walking ability. Using a walker may help patients who have more trouble walking. These measures usually improve pain and function. But arthritis is progressive. Even with treatment, it gets worse over time. Weight loss can help decrease stresses on all of the joints. If you are overweight, you should strongly consider losing weight.
Treatment Options: Surgical
Even when you get all of the right nonsurgical treatments, problems with pain and mobility sometimes get worse. In this case, the doctor may recommend surgery. Surgical options include:
Arthroscopy: Arthroscopy of the hip is a minimally invasive, outpatient procedure. It is relatively uncommon. The doctor may recommend it if the joint has evidence of torn cartilage or loose fragments of bone or cartilage.
Osteotomy: Candidates for osteotomy include younger patients with early arthritis, particularly those with abnormally shallow hip socket (dysplasia). The procedure involves cutting and realigning the bones of the hip socket and/or thighbone. This creates a more normal relationship between the ball and socket. It decreases pressure in the joint. In some cases, this may delay the need for replacement surgery for 10 to 20 years.
Traditional Hip Replacement: The doctor may recommend hip replacement when all of the above measures have been considered or have been tried and failed. Traditional hip replacement surgery involves making a 10-inch to 12-inch incision on the side of the hip. The muscles are split or detached from the hip. The hip is dislocated. The ball of the femur is removed. The hip socket is prepared by removing any remaining cartilage and some of the surrounding bone. The cup implant is pressed into the bone of the socket. It may be secured with screws. A bearing surface is inserted into the socket.
Next, the femur is prepared by removing some bone from the inside of the thighbone. A metal stem is placed into the thighbone to a depth of about 6 inches. The stem implant is either fixed with bone cement or is implanted without cement. Cementless implants have a rough, porous surface. It allows bone to adhere to the implant to hold it in place. A ball is then placed on the top of the stem. The ball-and-socket joint is recreated.
Minimal Incision Hip Replacement: Minimal incision hip replacement surgery lets the surgeon perform hip replacement through one or two smaller incisions. Compared with most people getting hip replacements, candidates for minimal incision procedures are typically thinner, younger, healthier and more motivated to have a quick recovery. Before you decide to have a minimally invasive hip replacement, get a thorough evaluation from the operating surgeon. Discuss with him or her about the risks and benefits. Both traditional and minimally invasive hip replacement procedures are technically demanding. They require that the surgeon and operating team have considerable experience.
The artificial implants used for the minimally invasive hip replacement procedures are the same as those used for traditional hip replacement. Specially designed instruments are needed to prepare the socket and femur and to place the implants properly. The artificial hip is implanted in the same way. But there is less soft-tissue dissection than with longer incisions.
A single minimally invasive hip incision may measure only 3-inches to 6-inches. It depends on the size of the patient and the difficulty of the procedure. The incision is usually placed over the outside of the hip. The muscles and tendons are split or detached, but to a lesser extent than in the traditional hip replacement operation. They are routinely repaired after the surgeon places the implants. This helps healing. It helps prevent dislocation of the hip.
Two-incision hip replacement involves making a 2-inch to 3-inch incision over the groin for placement of the socket and a 1-inch to 2-inch incision over the buttock for placement of the stem. To perform the two-incision procedure, the surgeon needs guidance from X-rays. It may take up to two or three times as long to perform this surgery, as it takes to perform traditional hip replacement surgery.
Reported benefits of less invasive hip replacement include:
• Less pain
• More cosmetic incisions
• Less muscle damage
• Rehabilitation is faster
• Hospital stays are shorter--For traditional hip replacement, hospital stays average four to five days. Many patients need extensive rehabilitation afterward. With less invasive procedures, the hospital stay may be as short as one or two days. Some patients can go home the day of surgery.
Early studies suggest that minimally invasive hip replacement surgery streamlines the recovery process. But the risks and long-term benefits of the less invasive techniques have not yet been documented to represent an improvement over traditional hip replacement surgery.
Research on the Horizon/What's New?
Extensive study and development are now underway to determine the long-term benefits of minimally invasive hip replacement. New technology for imaging and computer-assisted implant placement has been developed. It continues to be modified as experience with smaller incision surgery grows. This will allow more precise reconstruction of the hip with less direct visualization. In addition, new implant designs and materials are being developed to both facilitate minimally invasive surgery on the hip and to prolong the lifespan of replacements
Updated: 07/20/2007
Source: http://orthoinfo.aaos.org/
Reviewed by: Dr. Montesinos